Nasogastric tubes (NGT) are flexible tubes made primarily of plastic inserted through the nostrils and advanced through the nasopharyngeal tract and into the upper portion of the small intestine. These tubes serve several functions, including delivering food and nutrients to patients’ GI tracts, removing nasogastric contents, and assisting in lavage. Because of its invasive nature and the structure of the upper GI tract, the placement of NG tubes is best confirmed using X-rays.

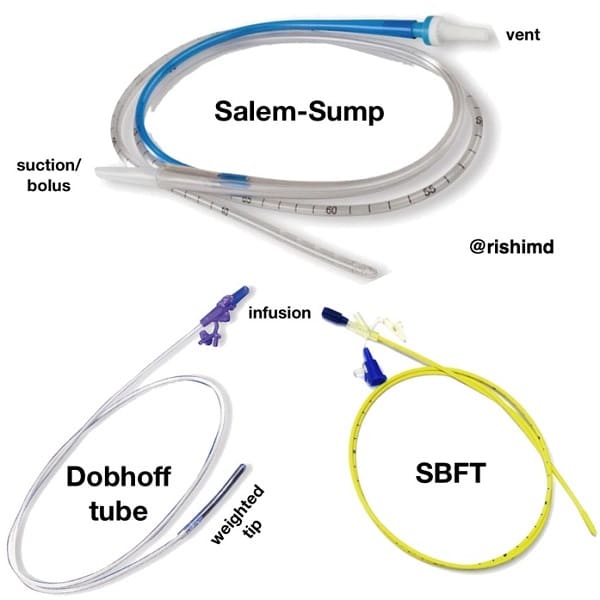
The nurse caring for a patient using an NG tube should keep in mind that the tube’s purpose should be clearly communicated, and if the patient requires several tubes to be inserted, these should be labeled appropriately. The following are the most common types of nasogastric tubes:
- Levin Tubes. Made of small-bore and single lumen tube that is generally used for administration of medications and feeding.
- Salem Sump Tubes. These tubes have a larger bore and double lumen. The first lumen is used to aspirate gastric contents, while the other lumen is used to relieve negative pressure in the GI tract and prevent the gastric linings from being drawn inside the catheter.
- Dobhoff Tube. This tube has a small bore and is characterized by the weight at the end of the tubing. The weight is used to help pull the tube in place via force of gravity.
Patients with NG tubes needed additional care requisites to help ensure that the tube stays in place and the goals of care are met. Nurses need to note the following in providing care to the patient with an NGT:
- Ensure comfort of the patient since the tube can irritate the nasal mucosal linings.
- Secure the tube’s insertion site at the patient’s nose by using a micropore tape to prevent it from excessive movement, pulling or dragging.
- Ensure that the care plan for the patient includes mouth care because mouth breathing relative to the presence of the tube in the nares. This is done to help prevent dryness and cracking of the lips.
- For patients who are still able to swallow, advised to suck on ice chips several times daily to relieve mouth dryness.
- Assess and note for the presence of symptoms such as abdominal pain and spasms, nausea or vomiting and report it immediately to the physician.
- Ensure that the patient is positioned in a semi-upright position to decrease the risk of aspiration of gastric contents.
Insertion of the NGT
The following steps are followed in the insertion of the nasogastric tube and the rationale for each action.
| Procedure | Rationale |
| Perform hand hygiene and prepare all the necessary supplies for insertion. | Hand washing is one of the best methods to prevent infections. Preparing all the supplies necessary would also help in faster and more efficient implementation of the procedure. |
| Check doctor’s orders for the type of NG tube to be placed and the reason for placement. | Check appropriate orders relevant to patient safety. |
| Check doctor’s orders to determine whether the NG tube is attached to suction or a drainage bag. | This should be commensurate with the reason for the NG tube. |
| Inspect the condition of the patient’s nasal and oral cavities, carefully noting for the presence of skin breakdown and lesions. | A visual inspection helps the nurse to determine which insertion site would be best to use and other precautions during the procedure. |
| Assess the patient’s level of consciousness and understanding of the procedure. | Patient must be able to follow instructions related to NG insertion to allow for the passage of the tube through nasal and gastrointestinal tracts. For unconscious patients, ensure that the caregiver is present and explain the procedure. |
| Assess the patency of the nares by asking the patient to sniff and exhale through the nose.
Note: If the patient is unconscious, place a finger a few inches below the nares to feel the air coming out to determine nasal patency. |
This helps determine the nostril suitable to be used as an insertion site. If both nares are suitable, select the nostril that would be more accessible to the suction device. |
| Palpate patient’s abdomen for distension, pain, and/or rigidity—Auscultate for bowel sounds. | Document assessment findings and determine the appropriateness of NG tube insertion related to the reason for insertion and the patient’s physical assessment. |
| Position patient sitting up at 45 to 90 degrees (unless contraindicated by the patient’s condition), with a pillow under the head and shoulders. | This allows the NG tube to pass more quickly through the nasopharynx and into the stomach. |
| Raise bed to a comfortable working height. | This helps prevent biomechanical injury to the health care provider. |
| Agree on a signal the patient can use if they wish you to pause during the procedure. | This procedure can be anxiety-provoking and uncomfortable for many patients. Providing a means for the patient to communicate discomfort and a desire to pause during the procedure helps alleviate anxiety. |
| Place a towel on the patient’s chest and provide facial tissues and an emesis basin. | Nasal and oral secretions may be evident during the procedure. |
| Provide the patient with drinking water and a straw if the patient is not fluid restricted. | Sipping water through a straw helps to initiate the swallowing reflex and facilitate the passing of the NG tube. |
| Stand on the patient’s right side if you are right-handed and the left side if you are left-handed. | The dominant hand is preferable to insert the tube, while the non-dominant hand can be used to support during the insertion. |
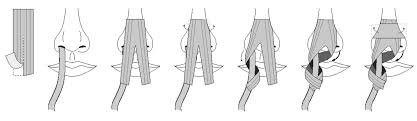
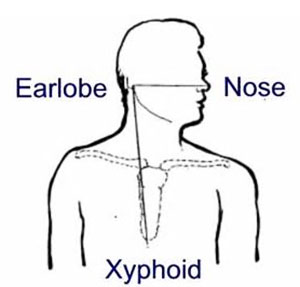
Measure distance of the tube from
and then mark the tube at this point.
|
This determines the appropriate length of the NG tube to be inserted. |
| Lubricate NG tube tip according to your agency policy. | The tube may be lubricated internally using tap water or externally using water-soluble lubricating jelly. Agency policy varies and should be checked.
Never use non-water-soluble lubricant (e.g., Vaseline), as it will not dissolve and may cause respiratory complications if it enters the lungs. |
| Apply clean non-sterile gloves. | Using gloves decreases the transfer of microorganisms. |
| Curve 10 to 15 cm of the end of the NG tube around your gloved finger, and then release it. | Curling the NG tube around your finger helps it conform to the normal curve of the nasopharynx. |
| Have the patient drop head forward and breathe through the mouth. | Dropping the head forward closes the trachea and opens the esophagus, which allows the NG tube to pass more quickly through the nasopharynx and into the stomach. |
| Insert NG tube tip slowly into the patient’s nostril and advance it steadily, in a downward direction, along the bottom of the nasal passage, with the curved end pointing downward in the direction of the ear on the same side as the nostril. | This follows the natural anatomical alignment of the nasopharynx. |
| A slight resistance maybe felt as the tune is advances along the nasal passage. Twist the tube slightly, apply downward pressure, and continue trying to advance the tube. If significant resistance is felt, remove the tube and allow the patient to rest before trying again in the other nostril. | It is common for the patient to feel discomfort, and this may be expressed with light coughing and gagging. More aggressive coughing and gagging may indicate that the tube has entered the airways, in which case you should withdraw the NG tube. |
| If there is difficulty in passing the NG tube, you may ask the patient to sip water slowly through a straw unless oral fluids are contraindicated. If oral fluids are not allowed, ask the patient to try dry swallowing while advancing the tube. | If the patient continues to gag or cough, check that the tube is not coiled in the back of the mouth, using a tongue blade and a flashlight to check the back of the mouth. If the tube is coiled, withdraw the tube until only the tip of the tube is seen in the back of the mouth. Then try advancing the tube again while the patient attempts to swallow. |
| Continue to advance the NG tube until you reach the mark/tape you had placed for measurement. | This ensures accurate placement. |
| Temporarily anchor the tube to the patient’s cheek with a piece of tape until correct placement can be checked. | This prevents displacement of the NG tube while checking placement. |
| Verify tube placement according to agency policy.
Color-coded pH paper is usually used, as an initial and interim check, to confirm that acidic contents are present. Then an X-ray is taken to confirm placement prior to using an NG tube for feeding. |
The contents aspirated from the tube should be acidic with a pH <5. If the pH is more than 6, it may indicate the presence of respiratory fluids or small bowel content, and the tube should be removed. |
| Once the tube placement has been confirmed, mark (with a permanent marker) and record the length of tubing extending from the nose to the outer end of the tube. | It aids in the timely recognition and identification of tube displacement or migration. |
| Secure the tube to the patient’s gown with a safety pin, allowing enough tube length for comfortable head movement. | This keeps the NG tube in place. |
| Document the procedure according to agency policy, and report any unexpected findings to the appropriate health care provider. | Timely and accurate documentation promotes patient safety. |
Care for the Patient During NGT Insertion
Patients receiving treatment with nasogastric tubes need to be repeatedly assessed for its placement and patency and the response to therapy. The following tips may help in ensuring effective use of the NGT as part of the treatment regimen:
- Ensure the placement and patency of the tube are assessed prior to feedings. Include in the assessment noting the location of the external markings and the color of the fluid aspirated from the tube.
- Never allow the patient to eat or drink anything without prior assessment of his swallowing reflex.
- Pin or tape the end of the tube to the patient’s gown to prevent pulling. Unpin it prior to changing the linens or use.
- Assess the patient immediately if the tube gets pulled out. Remember that it is not an emergency. Report the incident to the physician to determine whether there is a need to reinsert the tube.
- Note for any signs of respiratory distress and consider it as an emergency.
Removal of the NGT
The NGT should be removed as soon as the goals of the therapy are met and there is no longer a need for it. The process for removing the NGT is usually done very swiftly and without complications. However, prior to removing, check the physician’s order and see whether there is a need for ““trial”” clamping to determine the patient’s tolerance for its removal. Remember that symptoms such as nausea, vomiting, and abdominal distention should be noted during this period.
| Procedure | Rationale |
| Verify health care provider’s orders to remove NG tube. | An order is required to remove an NG tube. |
| Collect supplies. | Supplies include waterproof pads, a 20 ml syringe, tissues, non-sterile gloves, and a garbage bag. |
| Verify patient using two identifiers. Explain procedure to patient and place patient in high Fowler’s position. | Follow agency policy for proper patient identification. |
| Perform hand hygiene. Place waterproof pad on patient’s chest. | This reduces the transmission of microorganisms. |
| Disconnect the tube from the feed if present. | This prevents the risk of aspiration of tube feed. |
| Remove tape or securement device from the nose. | This allows for the tube to be easily removed. |
| Unclip the NG tube from the patient’s gown. | This allows for the tube to be easily removed. |
| Clear the NG tube by inserting 10 to 20 ml of air into the tube. | This prevents aspiration of tube feed from falling out of the tube. |
| Instruct the patient to take a deep breath and hold it. | This prevents aspiration; holding the breath closes the glottis. |
| Kink the NG tube near the naris and gently pull out the tube in a swift, steady motion, wrapping it in your hand as it is being pulled out. Dispose of the tube in a garbage bag. | This prevents any residual feed from flowing out of the tube upon removal. |
| Offer tissue or clean the nares for the patient and offer mouth care as required. | This clears the nares/nasal passages of any remaining secretions. |
| Remove gloves and place the patient in a comfortable position. Assess the patient’s level of comfort. Perform hand hygiene. | This promotes patient comfort and reduces the transmission of microorganisms. |
| Document procedure according to agency policy. | Document removal of NG tube and patient response to the removal. |
Common Nursing Diagnoses of Patients with NGT
Patients who are prescribed to have an NGT inserted may pose both actual and potential nursing problems due to the presence of the tube in their GI tract. Since NGTs are still foreign objects inserted into a patient’s body cavity, the nurse must ensure that the patient is carefully assessed and indications of health problems are addressed even before they cause other complications. The following are the most common nursing diagnoses seen among patients with NGTs:
- Pain-related to the accumulation of gastric fluids and/or abdominal distention secondary to accumulation of gas in the stomach
- Pain-related to the irritation of the pharyngeal mucosa secondary to insertion of the NGT
- Alteration in oral mucous membranes related to mouth breathing and NPO status
- Ineffective airway clearance related to the presence of a foreign object in the nasopharyngeal tract
- Altered nutrition less than body requirements related to NPO status
- Fluid volume deficit related to loss of gastric secretions and inability to take fluids orally
- Body image disturbance related to the presence of a foreign object in the nasopharyngeal tract
- Risk for aspiration related to the relaxation of the gag reflex secondary to the effect of the tube in place/use of oral anesthetic sprays
- Risk for excess fluid volume excess related to overfeeding of fluids/inability of the patient to utilize feeds fully.
- Risk for infection related to breaking in skin/mucous integrity
References
- Basavanthappa, B., (2015). Medical-Surgical Nursing. New Delhi: Jaypee Brothers Medical Publishers.
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Hinkle, J.L. & Cheever, K.H. (2018). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (14th ed.). Philadelphia: Wolters Kluwer.
- Morton, P., & Fontaine, D. (2018). Critical Care Nursing. Wolters Kluwer.
- Potter, P.A., Perry, A.G., Stockert, P.A., & Hall, A.M. (2019). Essentials for Nursing Practice (9th ed.). St. Louis: Elsevier.



![Caring for Patients with Tracheostomy and Nursing Diagnoses [ Updates] tracheostomynursingprocedure](https://rnspeak.com/wp-content/uploads/2020/10/tracheostomynursingprocedure_725820712-238x178.jpg)



