The Story of Mr. Timothy Brown and…2 more
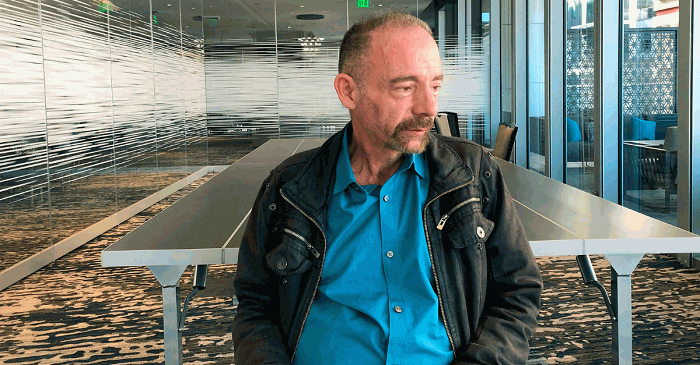
Mr. Timothy Ray Brown, known in the scientific world as the “Berlin Patient”, had been living with HIV. When a life-threatening opportunistic infection caused by the said virus, Acute Myeloid Leukemia (AML) struck him, his doctors were prompted to perform Bone Marrow Transplant to cure the blood cancer and save his life. However, the AML relapsed after a few months resulting in another BMT for the patient. Luckily for Mr. Brown, the painful experiences from the complex procedures he underwent to gain a cure from AML proved even better for him. It defeated not only his cancer but also his HIV/AIDS.
It has been 12 years since the story of the American-born, who has stopped taking his antiretroviral drugs after recovering from his BMT Procedure, rang loudly in the health community and across the globe for being the first man to have been officially “cured” from HIV.
Now, after long years of silence on HIV/AIDS cure-related news, it seems that 2019 ushers new hope for people living with HIV and everyone in-fear of the virus.
In a recent science conference in Seattle, USA, scientists announced that another possible cure may have been achieved in another HIV positive individual. From the likes of the first appellation, they call him the “London Patient”. Still unknown or anonymous, this person has been declared to have no traces of HIV in his body for 18 months since his first and last Bone Marrow Transplant. BMT was done because he developed Hodgkins Lymphoma, another form of blood cancer.
Despite the hesitation of others to fully declare him cured given the relatively short duration, clinical studies prove that it only takes weeks for HIV to come back after a person stops his/her anti-HIV drugs – leading many to hope high for the future of HIV cure.
But, the “London Patient” isn’t the last buzz of the matter, as other media outlets are leaking about another patient who underwent the same procedure and now also has no HIV traces in his blood. This news however is still hovering around waiting for further updates, as it’s only been 4 months since he last took his anti-HIV meds.
The History of HIV
The Human Immune Deficiency Virus (HIV) as a dreaded virus may seem like a late human discovery, appearing in the limelight only in the latter half of the 20th century – 1959 to be exact – as the year it was first known to infect a man in the Democratic Republic of Congo, Africa.
In the 2010 Progress Report of the World Health Organization (WHO) about HIV/AIDS, around 35 M people are infected with the immune system-targeting virus. This heavily stigmatized virus was discovered by scientists to have mutated from a different strain (Simian Immunodeficiency Virus) found in a subspecies of chimpanzees native to west equatorial Africa. Man acquired it through exposure to their blood from hunting.
In 1981, the first case of the full-blown Acquired Immune Deficiency Syndrome (AIDS) was documented and discovered to be blood-borne and sexually transmitted. From the trend of being common among young gay men and needle-using drug abusers, it was first named “Gay-related Immune Deficiency Cancer or simply Gay Cancer” but was later changed.
By 1983, the WHO, seeing the cases rise rapidly across continents and countries declared HIV/AIDS an epidemic. This was followed by a clinical trial of the first drug administered to HIV/AIDS infected individuals in 1986 that proved the drug Azidothymidine (AZT) was effective in reducing either death or the rise of opportunistic infections among the HIV-infected people. Despite this, by 1995, the disease has gained momentum as the leading cause of death for Americans at the age of 25 to 44 years old.
In addition, according to statistics, 97% of people now living with HIV come from poor to low-income countries specifically Sub-Saharan Africa where universal coverage is still far from the target. Progress has been made but there is more to be done.
The Current Progress in Treatment
Many countries, international organizations, governments, and even private entities in the battle against a rapid spreading virus have made progress. But there is more to know and discover about the enemy cum invader. Before the story of the “Berlin and London patients”, hope for a cure among the general public had been cloudy that fear and social stigma made it even more difficult to reach everyone. With infection rates growing faster than diagnosis and administration of treatment, a global health emergency is definitely called for.
However, development in spreading awareness, control and treatment is ongoing. Understanding the virus is paramount. And scientists are definitely trying their best to understand the virus and how it could possibly mutate further in the future.
According to experts, the secret to fighting AIDS is in stopping the replication of the virus within a person’s body. The HIV virus does not invade everywhere upon entry in the bloodstream. Just like a lock and key, it can only infect if it can get inside a specific cell called CD4 T cells. These are responsible for proper immune system functioning. If invaded and their insides altered, they can no longer function the way they should.
Luckily for all mankind, there are some people in the world considered virtually immune to HIV. Those with mutations in their CD4 Cells where a molecule called CCR5 supposedly present on the surface of the said cell, is absent in theirs. Without the CCR5, the virus has no gateway towards the cells’ insides and thus cannot invade and infect them. However, according to studies, only around 1% of Caucasians from Northern and Western Europe have these genetic mutation called: CCR5delta 32 homozygosity, which comes from both parents having the same gene.
Connecting the dots, it is not the BMT per se that cured the HIV positive patients, but the source of the bone marrows which are, for both the Berlin and London patient, from people with CCR5delta 32 homozygosity, or those with known immunity to the virus that causes AIDS.
However, the procedure for BMT is not as easy as other common procedures. Its three phases include the pre-transplant phase, the immediate post-transplant phase, and the late post-transplant phase.
For the pre-transplant phase, the kind of transplant to be done as well as the donor is identified. This involves a series of tests and procedures for both donor and donee. The recipient is then admitted into a unit where the administration of chemotherapeutic drugs and irradiation therapy is done to ensure that his/her body does not reject the donor’s bone marrow. These can lead to side effects related to the weakening of the body’s immune system. Loss of hair isn’t even the worst part. There can be loss of appetite, nausea, vomiting, bruising, feeling of tiredness among others. Some people may not be strong enough to go through these especially HIV/AIDS patients already ill.
The 2nd or immediate post-transplant phase includes the transplant itself, the immediate or acute reactions to the transplant and more chemotherapy and irradiation regimes for the patient.
The last or the late post-transplant involves managing the long-term suppression of the immune system until the body of the recipient can fully adapt to the otherwise foreign cells. This stage is the longest and also crucial. More drugs and monitoring are crucial especially that the patient is already discharged from the facility and just comes back for regular visits.
As a disease that affects not only the physical but also the psychological aspect of life, the role of nurses in HIV/AIDS management is quite crucial.
The Role of a Nurse in HIV/AIDS Treatment
Nurses play multiple roles in a patient’s life regardless of diagnosis or disease. A nurse theorist posited that nurses should focus more on a patient’s individual reaction or response to a disease rather than the disease itself. He/she is tagged as client-centered not disease-centered. As such he/she should first assess a patient’s physical, cognitive, psychological, and emotional condition rather than just provide a series of interventions based on the book. Aside from these, a nurse must keep up to date with the current trends in treatment to effectively perform his/her function.
For example, the current trend of treatment of HIV AIDS include:
- Possible shifting of daily medication administration to once a month injection of 2 combination drugs – Cabotegravir and Rilpivirine in the near future.
- Engineering proteins in the laboratory to optimize inherent antiviral proteins.
- Bone Marrow Transplant from donors with a CCR5delta 32 homozygosity gene mutation to cure HIV.
- Alteration of HIV genes to weaken the virus’ ability to infect cells.
Along with these trends, nurses usually play as:
- Health Educators to spread awareness about HIV/AIDS and Working to erase the social stigma that induces fear and misunderstanding.
- Role Model of Safe Health habits such as the practice of universal or standard protection (i.e. basic handwashing and use of PPEs)
- Watch guards by avoiding accidental pricks from sharp instruments used for HIV positive patients, proper labeling of items such as blood of patients with HIV/AIDS, proper cleaning of spilled blood, isolation of sharp items used by and for HIV patients and practice of correct needle disposal.
- Confidante/Counselor. The diagnosis of HIV and especially AIDS may put a lot of stress on a person. Thus, he/she may need someone to share his fears, doubts and pains. The nurse as the front liner must know how to handle these.
- Primary Care Provider As a primary care provider, a nurse may administer medications; perform physical and psychological tests, assist in physical mobilization as well as other healthcare needs.
Further on, in the management of all STDs, there are Four (4) Cs used by health providers. The first one is counseling and education or giving information about the kinds of STDs including HIV and how it can be prevented in others. Next is, the use of Condoms. Proper use of condoms is advocated in the prevention of STDs. The third is compliance with treatment. Nurses should be able to explain properly the importance of completing treatment. Lastly, contact tracing especially partners for treatment. This helps prevent further spread of infection.
Must-Know:
HIV and AIDS are somewhat distinct in meaning. HIV means Human Immune Deficiency Virus, the virus that infects a person’s immune system and weakens it by killing CD4 cells, one of the cell types responsible for regulating the body’s immune responses. On the other hand, AIDS is a collection of potentially fatal illnesses and cancers that cannot be fought by an HIV patient’s compromised immune system.
References
- HIV and AIDS: An Origin Story. www page. Accessed March 22, 2019. https://www.publichealth.org/public-awareness/hiv-aids/origin-story/
- Alcorn, K. (2010, December 13). Stem Cell Transplant has Cured HIV infection in “Berlin Patient”, say doctors. www page. Accessed March 20, 19 http://www.aidsmap.com/page/1577949/
- World Health Organization. (2010). Towards Universal Access: Scaling up priority HIV/AIDS Interventions in the Health Sector.
- https://www.who.int/hiv/pub/2010progressreport/summary_en.pdf?ua=1
- Global Report: UNAIDS report on the global AIDS epidemic 2013. http://www.unaids.org/sites/default/files/media_asset/UNAIDS_Global_Report_2013_en_1.pdf
- HIV update – 21st March 2019. www page. Accessed March 19, 19 http://www.aidsmap.com/page/3469181/
- The Aids Institute. Where did HIV come from? www page. Accessed March 19, 2019 https://www.theaidsinstitute.org/education/aids-101/where-did-hiv-come-0
- Fred Hutch: Cures Start Here. Understanding HIV’s Evolutionary Past – and future. (2017, November 20). Tompa, Rachel. www page. Accessed March 20, 2019 https://www.fredhutch.org/en/news/center-news/2017/11/hiv-evolutionary-past-and-future.html
- Fred Hutch: Cures Start Here. London Transplan Doctors report 2nd person likely cured of HIV. www page. Accessed March 19, 2019.https://www.fredhutch.org/en/news/center-news/2019/03/hiv-cure-timothy-brown.html
- Holmes, W. Preparing the Patient for Bone Marrow Transplantatio: nursing care issues, www page. Accessed March 20, 2019
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2589372/?page=2