The influx of patients affected by novel coronavirus has reached unprecedented levels causing a shortage of hospital beds, particularly negative pressure rooms and Intensive Care Unit beds. Drastic measures are being taken to repurpose facilities in catering to the colossal amount of flooding suspected and infected cases worldwide. The relentless climb of infections that spread like a wildfire and the average hospital length of stay of patients affected by COVID-19 can knock down the entire hospital including its workforce for a short period of time.
The Disease Process
COVID-19 develops flu-like symptoms such as fever, headache, dry cough, myalgia, nausea, fatigue, and abdominal discomforts with diarrhea, anorexia, anosmia on day 2-11 (with an average of 5 days) post-exposure. On day 5, the patient likely develops bilateral viral pneumonia resulting in shortness of breath or dyspnea. Day 10, leads to cytokine storm causing acute lung injury and eventually multi-organ failure in approximately 4-5 days. The fifth day onwards after contracting the disease is considered the most crucial days due to poor prognosis and slow recovery as there is no specific treatment to prevent or treat the virus. Infected patients are rendered with supportive and palliative care to alleviate the symptoms during the course of illness. The patient’s response to supportive treatment will determine the prognosis of the disease.
The Hospital Bed Turn-Over Rates
Hospital length of stay will increase due to slow recovery and disposition issues related to the transmission of infections when the patient is dischargeable to home.
In the study of Guan (2020), the median hospital length of stay for COVID-19 acute and critical cases was 12.0 days with a mean of 12.8. The incubation period of Coronavirus disease from publicly reported confirmed cases was estimated 2-14 days after contracting the illness. Neuman and colleagues (2020) projected 5 days expected length of stay (LOS) for simple pneumonia with pleurisy in adults while 7-10 days for patients with severe pneumonia involving ICU admission. However, in a comparative study on survivors versus non-survivors showed that patients with Acute Respiratory Distress Syndrome (ARDS) who underwent ICU admission were discharged after 22 days from the day after illness onset, while non-survivors who suffered from complications such as sepsis, acute cardiac injury, acute kidney injury and secondary infection died on the 18-19th day.
According to WHO (2020), a survey based on the largest cohort of COVID-19 outbreaks showed an approximately 40% of patients are mild cases which do not require hospital admission; about 55% (40% moderate cases + 15% severe cases) requires inpatient care, and more or less 5% are critically ill requiring ICU admission. However, statistics vary demographically and will depend on the country’s advancement in the healthcare system and technology.
The data implies a ZERO hospital bed turnover rate for symptomatic patients during the course of 14 days incubation period due to treatment and isolation requirements, and an additional one-week duration for severely affected cases. 60% of the population affected by the virus can block the entire hospital for 1-3 weeks. The outbreak aggravated the condition as the cases upsurge to doubling rates every 3 days making hospitals reached its tipping point.
The Delays and Waiting Time
Screening plays a vital role in case finding, early detection, early diagnosis, and prevention of transmission. A PCR test takes only 6 hours from start to finish however, as the demands grow ─ testing kits unavailability and laboratory workforce shortage caused backlogs. Delays on test results may reach up to 7 days means delays in case identification.
The upsurge of COVID-19 suspected cases overwhelms the healthcare system resulting to spread of infections, mismanagement of workforce, misuse of medical resources, and poor hospital bed utilization. The standstill period while waiting for the laboratory result may not only prolong the agony but failure on early detection of positive cases may jeopardize infection control efforts, and compromises the public health objectives and safety of the healthcare workers. The daily out-turn cost of waiting time for patients with negative results means mismanagement on the workforce and misuse of medical resources which are intended for patients affected by the virus.
Case Management Approached on Transitional Care for COVID-19 Cases
The Case Management Approached in the care of COVID-19 patients is a multidisciplinary system designed to attain the following goals:
- Lessen hospitalization length of stay, thus improving bed utilization and higher turn-over rates
- Faster and safe delivery of care from admission to discharge through proper utilization of medical resources
- Early discharge of patients without compromising public health objectives
- Prevention of complications from prolonged hospital confinement including the spread of infection and acquiring nosocomial co-infections
- Continuity of care initiated at community facility admission, inpatient care and after discharge follow-ups; and lastly,
- Prevention of readmissions.
This will strengthen the collaborative works of infection control management, home health care, community health care, and hospital care settings.
Transitional Care Model in the management of COVID-19 promotes the safe and timely transition of patients between levels of health care and across care settings. The TCM ensures the continuity of care between the hospital’s in-patient care and community-based settings, such as homecare quarantine and patient-centered medical community facility throughout the course of acute illness.
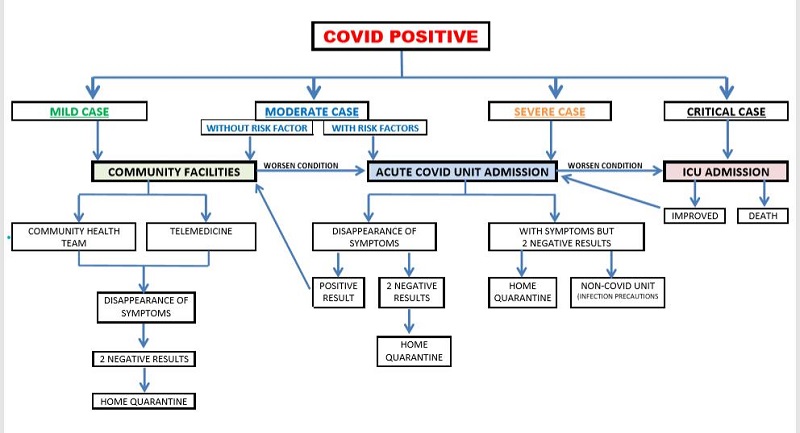
Transitional Levels of Care According to Category
WHO (2020) categorized patients according to the severity of the disease such as; mild (symptomatic treatment and does not require inpatient care), moderate (requires admission for inpatient care), severe (requiring admission for close monitoring and oxygenation therapy), and critical (requiring ICU admission for mechanical ventilation and life-saving support).
Note: In obtaining 2 consecutive negative results, pls. see CDC Guidelines, 2020.
Only confirmed COVID-19 positive cases will be admitted to the designated COVID facility. COVID community facility can be a repurposed institution or hotels which will be managed by the community health care team or via telemedicine. COVID referral hospitals should have a designated Acute COVID Unit and an Intensive Care Unit. COVID patients discharged to home should follow the quarantine protocols and follow up by the home health care team or community health care team. Home quarantine with strict infection control precautions should be observed after discharge due to reports of possible post convalescent viral shedding as seen on 22 days of respiratory tract samples and from faeces of affected patients between two weeks and more than one month after contracting the disease.
References:
- Guan, W.J., Ni, Z.Y., Hu, Y., et. al. (2020). Clinical Characteristics of Coronavirus Disease 2019 in China. The New England Journal of Medicine.DOI: 10.1056/NEJMoa2002032 Lauer, S.A., Grantz, K.H., Bi, Q., et al. (2020). The Incubation Period of Coronavirus
- Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases:Estimation and Application. Annals of Internal Medicine.DOI: 10.7326/M20-0504 Neuman, T., Damico, A., & Cubanski, J. (2020). How Much Could Medicare
- Beneficiaries Pay For a Hospital Stay Related to COVID-19? Kaiser Family Foundation: Retrieved on 04 April 2020 from https://www.kff.org/medicare/issue-brief/how-much-could-medicare-beneficiaries-pay-for-a-hospital-stay-related-to-covid-19/ Zhou, F., Yu, T., Du, R., et. al. (2020). Clinical Course and Risk Factors for Mortality of Adult Inpatients with COVID-19 in Wuhan, China: A Retrospective Cohort Study. The Lancet, 35(10229), pp. 1054-1062. DOI:https://doi.org/10.1016/S0140-6736(20)30566-3 Lewin, E. (2020). Clinical Course of COVID-19: What GPs Need to know?
- NewsGP: The Royal Australian College of General Practitioners (RACGP)Retrieved on 04 April 2020 from https://www1.racgp.org.au/newsgp/clinical/clinical-course-of-covid-19-what-gps-need-to-know
- Appleby, J. (2020). What Takes So Long? A Behind-The-Scenes Look at The Steps Involved in COVID-19 Testing. Kaiser Health News. Retrieved on 04 April 2020 from https://khn.org/news/what-takes-so-long-a-behind-the-scenes-look-at-the-steps-involved-in-covid-19-testing/
- World Health Organization. (2020). Operational Considerations for Case Management of COVID-19 in Health Facility and Community.Retrieved on 06 April 2020 from https://apps.who.int/iris/bitstream/handle/10665/331492/WHO-2019-nCoV-HCF_operations-2020.1-eng.pdf
- European Centre for Disease Prevention and Control. (2020). Novel coronavirus (SARS-CoV-2). Discharge criteria for confirmed COVID-19 cases – When is it safe to discharge COVID-19 cases from the hospital or end home isolation? Retrieved on 07 April 2020 from https://www.ecdc.europa.eu/sites/default/files/documents/COVID-19-
- Centers for Disease Control and Prevention. (2020). Discontinuation of Transmission- Based Precautions and Disposition of Patients with COVID-19 in Healthcare Settings (Interim Guidance). Retrieved on 07 April 2020 from https://www.cdc.gov/coronavirus/2019-ncov/hcp/disposition-hospitalized-patients.html