Accurate documentation is crucial in the nursing profession, as it is the foundation for providing safe and effective care to patients. This responsibility not only ensures legal compliance but also plays a significant role in the daily work of nurses. The common term used in the field of nursing when it comes to documentation is charting. Though nurses may fill up many forms each working day, the most integral part of the nurses’ responsibility is charting.
Brief History of Charting
From clay tablets to computer screens, charting has come a long way in documenting a patient’s medical history. Here’s a quick trip through this evolution:
Ancient Beginnings (Before 3000 BC):
Early Records
Even in prehistoric times, medical observations were etched on cave walls or clay tablets. These were primarily for tracking illnesses and treatments.
Papyrus and Parchment (3000 BC – 1400 AD):
Egyptians and Greeks: The Egyptians used papyrus for medical scrolls, while the Greeks adopted papyrus and later switched to parchment. These documents recorded symptoms, treatments, and prognoses.
The Book Age (1400 AD – 1800 AD):
Paper and Printing Press: The invention of paper in China and the printing press by Gutenberg revolutionized record-keeping. Medical journals and textbooks emerged, allowing for wider dissemination of knowledge. Physician Notes: Doctors kept detailed handwritten notes on individual patients in bound volumes.
The 20th Century Shift (1800 AD – 1990s):
Standardized Forms: The 20th century saw the rise of standardized medical charts with specific sections for demographics, medical history, medications, allergies, etc.
Dictation and Typing: Physicians began dictating notes for transcription by secretaries, leading to more detailed records.
The Digital Age (1990s – Present):
Electronic Health Records (EHRs): The rise of computers brought Electronic Health Records (EHRs). These digital systems allow for faster data entry, easier access to information, and improved communication between healthcare providers.
Integration and Mobility: Modern EHRs integrate with various medical devices and lab results, providing a more comprehensive patient picture. Mobile access for doctors and patients is also increasing efficiency.
Purpose of Charting
The purpose of charting is multifaceted. From tracking the progress of a patient’s condition to being utilized as a valuable tool in research, listed below are the different purposes of charting.
- Charting serves as a permanent record. Charting means documenting a patient’s entire healthcare journey from admission to discharge. This record captures vital information that is essential for healthcare providers to track the patient’s condition, treatment progress, and outcomes. By having access to this information, healthcare professionals can make informed decisions and maintain continuity of care.
- Charting tracks Progress. Charting enables healthcare providers to monitor the patient’s condition, treatment progress, and outcomes, facilitating informed decision-making and continuity of care.
- Charting holds legal significance. It acts as evidence in the event of complaints or malpractice claims, providing a detailed account of the care provided and the patient’s response. This documentation ensures accountability and transparency in the nursing profession.
- Charting ensures continuity of care. By documenting interventions, assessments, and changes in the patient’s condition, subsequent caregivers have a reference to provide seamless care. This documentation allows for better coordination and communication among healthcare providers.
- Charting serves as a valuable tool for research purposes. It provides retrospective data that enables healthcare professionals to analyze trends, outcomes, and the effectiveness of interventions. This information contributes to the advancement of medical knowledge and improves patient care.
Types of Charting
- Narrative Charting
This is the traditional form of charting. It is a source-oriented record wherein each medical personnel makes documentation on the patient’s record in a separate section. The advantage of using this type of recording is the provision of organized sections for each member of the healthcare team. The disadvantage of using this type of recording is that the information is scattered throughout the chart. A review of history and accurate endorsements must be done in this type of charting.
Examples:
Treatment Chart
Admission sheet
Initial Nursing Assessment
Graphic Record
- Problem-oriented medical record
Introduced by Lawrence Weed in the 1960s, the Problem-Oriented Medical Record (POMR) focuses on patient problems rather than chronological events. This approach promotes collaboration among healthcare professionals by emphasizing:
Problem List: A comprehensive compilation of the patient’s existing medical issues.
Plan of Care: A documented strategy shared among healthcare providers to address each problem.
Progress Notes: Updates that reflect the patient’s response to interventions and any changes in their condition.
Advantages:
- Encourages teamwork and communication among healthcare providers.
- Provides a clear and focused view of patient care goals.
Disadvantages:
- Requires an accurate and comprehensive initial problem list.
- Maintaining the record can be time-consuming, especially in complex cases.
Contents of Progress Notes
1. SOAP formats –This format is commonly used since it gives a quick look at the observation of each nurse as well as the nursing action on each observation.
S – Subjective data includes the patient’s complaints or perception of the present problem stated.
O – Objective data includes the nurse’s observation using his or her clinical eye and data gathered from measurements.
A- Assessment (In some books and methods, this is also called analysis). Following the collection of both subjective and objective data, the nurse should assess the patient’s condition and determine any appropriate nursing diagnoses.
P – The plan includes the nursing actions to be made to solve the stated problem. This part of charting can be revised.
Some SOAP formats include interventions, evaluations, and revisions (SOAPIER).
I – Intervention –This is the part wherein specific nursing actions are stated
E – Evaluation –This is the part wherein the nurse evaluates the reaction of the patient or the progress of the problem being solved.
R-Revision – This is the section that states the changes made to further resolve the problem.
Example:
Case: A patient with hypersensitivity reaction secondary to food intake.
S – “My skin is so itchy, especially on the skinfolds.”
O – Skin appears to be flushed with bumps. Irritation was noted on the armpit and inner thighs.
A – Altered comfort secondary to food intake
P – Inform the patient not to scratch the skin.
– Apply a cold compress on the hot spots
– Cut nails to prevent skin scratches
– Refer to the physician
-Assess for the progress of skin rash
I – Instructed not to scratch the skin.
-Cut the fingernails short
-Applied cold compress
–Referred to the physician
E – “I feel more comfortable and I do not have the urge to scratch my skin.”
R – Give antihistamine (Antamin) 1mg/mL as a deep intramuscular injection to the left deltoid muscle.
2. Focus Charting – This type of charting involves Data, Action and Response category. This is a client-focused charting. This form reflects a holistic approach to the client’s needs since the client is the main focus of the documentation.
Data. The data section contains details, about the client’s situation, such, as their history, current symptoms, assessments, and relevant observations.
Action. The action part describes the steps or treatments implemented based on the data gathered, which could involve administering medications providing treatments, or sharing resources with the client.
Response. In the response segment we record how the client reacted to these actions – did their condition get better? Did they face any side effects? This documentation helps evaluate the effectiveness of the interventions. By emphasizing these three components DAR charting presents a brief overview of the client’s development while ensuring that their care plan is customized to meet their requirements.
Example:
D – 7:30 am Patient received via wheelchair, with guarding behavior on head and nape, Facial grimace noted, graded the nape pain as 7 on a scale of 1 to 10 with 10 as severe pain.
A – assessed condition monitored vital signs; gently massaged neck and shoulders; 8:00 am given Norgesic Forte per orem as ordered.
R – 3:00 pm verbalized pain is reduced and rated pain as 2/10; able to walk on her own.
3. Charting by Exception (Checklists and Flowsheets)
CBE offers an alternative to detailed notes. It focuses on recording only deviations from a patient’s expected condition. This saves nurses significant time, allowing them to devote more attention to other tasks.
However, while it has its fans, CBE also has limitations. First, it requires a clear understanding of a patient’s “normal” baseline. Since each healthcare facility defines “normal” differently, these definitions might not always match a specific patient’s situation. For instance, a liver transplant recipient may never have bilirubin levels within the standard range. Second, CBE can omit valuable details, making it difficult to track a patient’s progress or verify if procedures were performed.
The way CBE works can vary depending on the healthcare setting’s documentation tools. Facilities often use checklists and flowsheets to streamline information gathering. Nurses simply check boxes or put initials on these forms, allowing them to move on to the next patient quickly.
Checklists and Flowsheets
Checklists and flowsheets used in different health departments are examples of charting by exception. These pre-designed templates, typically one or two pages long, list all the relevant data points, services, and measurements for a specific patient visit, assessment, or condition. Mainly consisting of checkboxes and short blank spaces, they’re faster and easier to complete than writing lengthy narratives. In addition, the standardized format simplifies comparisons across visits and helps identify any abnormalities in the patient. For example, a standard admission form with vital signs at the top would readily show changes in weight or blood pressure compared to previous visits.
While flow sheets and checklists are efficient, they can’t capture everything. These forms provide limited space thus provide a brief glimpse into the patient’s situation. Because of this, they’re usually used alongside other, more detailed charting methods, not as a complete replacement.
Both checklists and flowsheets can be used for charting by exception (CBE), but they serve slightly different purposes:
Checklist
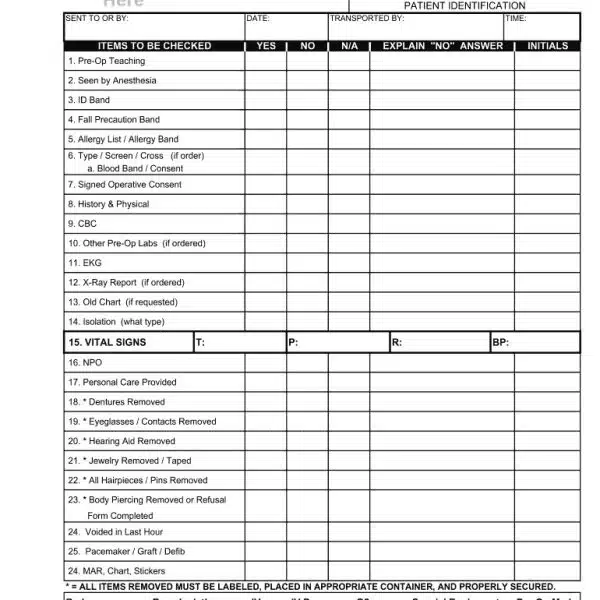
Focus: is a list of specific items or tasks.
Content: Includes expected findings or actions. A checkmark indicates something is normal or completed while leaving it blank suggests a deviation.
Uses: Suitable for situations with a defined set of criteria to assess or procedures to follow.
Example: A pre-operative checklist might include confirming patient NPO status (nothing by mouth), verifying allergies, and ensuring informed consent is obtained. A checkmark beside each item signifies normalcy, while a blank space prompts further documentation.
Flowsheet
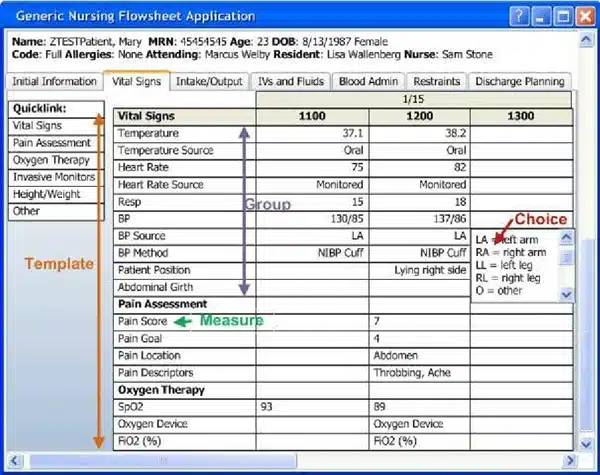
Focus: A sequential chart tracking ongoing assessments or interventions over time.
Content: Has designated spaces for recording specific data points at regular intervals. Deviations from normal ranges are typically highlighted or require additional comments.
Uses: Ideal for monitoring trends or changes in vital signs, pain levels, intake/output, or medication administration.
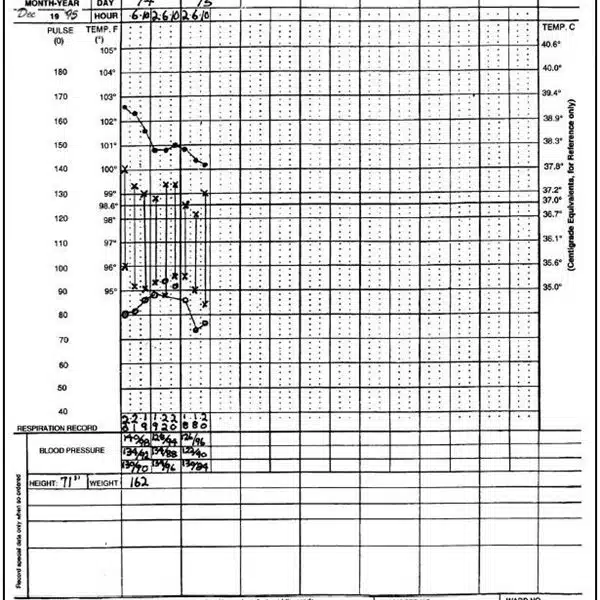
Example: A vital signs flowsheet might have columns for temperature, heart rate, blood pressure, and oxygen saturation recorded every four hours. A significant rise in temperature would be flagged for further investigation.
Guidelines in charting for nurses
1. Make every entry precise.
As a nurse, precision is the key to clear understanding between colleagues as well as the legalities that surround the charting. Being precise means being specific when it comes to describing the observations done, on the other hand, being accurate must also give factual and measurable units. The accuracy also involves the time element which is an important part of sequencing the events.
2. Be objective.
Objectivity is vital in nursing documentation. Nurses are trained to record factual observations, avoiding personal opinions or hunches. This means separating emotions from assessments, ensuring transparency and clear communication of patient events throughout their care.
3. Write legibly (print is preferred).
Clear and concise documentation ensures everyone involved in the patient’s care, including quality assurance personnel, can easily understand the information. You cannot write in a script other than in the signature section. This shows that you are the one who assumed the patient’s responsibilities and recorded the kind of care the client received. Remember, nursing terminology should be accurate and precise to effectively communicate the patient’s condition and the holistic care provided.
4. Ensure that charting is complete.
When charting, always follow the nursing process. Charting should reflect the assessment, planning, implementation, and evaluation phases of patient care. Document all relevant information such as vital signs, medications administered, patient responses, treatments performed, and any changes in condition. Remember, in nursing, when an intervention is not documented, it means it was not done.
5. Be timely.
Chart entries should be made promptly. Documenting care as soon as possible ensures accurate recall and avoids confusion. Date and time should always be entered because it is crucial for tracking the progression of a patient’s condition.
6. Be clear and concise.
Use standard medical terminology. This promotes clear communication among healthcare professionals. Avoid jargon and unfamiliar abbreviations which could lead to confusion. Organize your entries logically to make it easier for others to understand the flow of care.
7. Document errors and omissions.
Explain what happened, and what actions were taken to rectify the situation, and notify the appropriate personnel.
8. Never chart something you didn’t do
This is a serious offense and can have legal repercussions. Inaccurate record keeping can pose risks, to safety. When healthcare providers depend on incomplete information in charts it can result in errors in medication administration incorrect treatment plans and delays in diagnosing conditions. Precise documentation helps shield healthcare professionals from liabilities if a situation escalates to a lawsuit. If there are issues, with a patient’s care and the recorded information is inaccurate it might be utilized as proof that works against you.
9. Refrain from copying other charting.
In healthcare, providing the highest quality care hinges on a thorough and individualized understanding of each patient. This means conducting your comprehensive evaluation, even when there are existing charts from colleagues.
Every patient brings a distinct medical history, current concerns, and overall health picture. By performing your own assessment, you gain a firsthand perspective on their specific situation, ensuring you don’t miss any crucial details.
Remember, your documentation should always reflect your own findings and clinical judgment. By taking ownership of your assessments, you’re not only fulfilling your professional responsibility but also contributing to a higher standard of patient care for everyone involved.
In conclusion, charting emerges as the bedrock of responsible and exceptional nursing practice. It serves a multitude of purposes, from safeguarding patient well-being to ensuring legal accountability. By meticulously documenting patient information, nurses contribute to:
Key Takeaways
Charting emerges as the bedrock of responsible and exceptional nursing practice. It serves a multitude of purposes, from safeguarding patient well-being to ensuring legal accountability.
Charting offers a multitude of benefits:
Comprehensive Care: Detailed records paint a complete picture of the patient’s journey, facilitating informed decisions by the healthcare team.
Continuity of Care: Clear documentation ensures a smooth handover of patient information between healthcare providers.
Legal Protection: Objective charting serves as a vital defense mechanism in potential legal situations.
Research and Improvement: Data from charting fuels valuable research that improves healthcare practices.
Nurses employ various charting methods:
Narrative Charting: This traditional method features separate sections for each healthcare professional’s observations.
Problem-Oriented Charting: This method focuses on patient problems, with healthcare providers collaborating on a plan of care. SOAP (Subjective, Objective, Assessment, Plan) or SOAPIE (Intervention, Evaluation) formats are commonly used for progress notes.
Focus Charting: This client-centered approach documents data, actions taken, and patient responses.
Beyond the method employed, adherence to key principles is also important to produce quality charting.
In conclusion, meticulous and accurate charting is the cornerstone of exceptional nursing practice. It safeguards patient well-being, ensures legal accountability, and contributes to improved healthcare outcomes. Mastering various charting methods empowers nurses to deliver holistic and effective care for every patient entrusted to their care.
References
- De Groot, Kim et al. “Nursing documentation and its relationship with perceived nursing workload: a mixed-methods study among community nurses.” BMC nursing vol. 21,1 34. 28 Jan. 2022, doi:10.1186/s12912-022-00811-7
- Berman, A., Kozier, B., & Erb, G. L. (2012). Kozier and Erb’s fundamentals of nursing (2nd ed). Pearson Australia.
- Nurse, Natasha MS, RN. Charting Nursing’s Future. AJN, American Journal of Nursing 116(9):p 61,62, September 2016. | DOI: 10.1097/01.NAJ.0000494698.93863.b9







![FDAR Charting for Nurses [5 Tips for Effective FDAR Charting & Common Mistakes to Avoid] Fdar charting](https://rnspeak.com/wp-content/uploads/2023/06/Fdar-charting-238x178.jpg)





REQUESTING FOR MORE CHARTING TO BE PUBLISHED!THANKS A LOT!
GENUINELY EXCELLENT!