Summer season has now lapsed and rainy days are setting in the Philippines as a tropical country is included to the Center for Disease Control and Prevention list for one which has dengue outbreaks for the past years. According to the statistics, there were 126,000 dengue cases in the country last 2011. Thus, recently the Department of Health (DOH) strictly encourages the public citizens to continue and strengthen their fight against dengue. Today, the goal of the DOH according to Dr. Eric Tayag is to decrease the number of dengue cases to at least 100,000 cases comparative to last year’s figures.
There was a slight gist of hope for all since DOH has reported an 8.52% decline in dengue cases last January 1 to May 5 of this year; compared to the growth of cases last year on the same said period. Nevertheless, we should not be at ease of this since the peak season of dengue fever is still somewhere between the months of July and August. So, here are the things we should know about dengue hemorrhagic fever and its corresponding nursing care management.
Dengue hemorrhagic fever is caused by a bite of a vector mosquito called, Aedes Aegypti. This mosquito is considered to be a day- biting and low flying mosquito and commonly be found inside the household. On the other hand, some reports initiated by a study in the UP Los Banos had produced another suspicious mosquito to be a dengue carrier- known as Aedes Albopictus. This time, this said mosquito is a night biting mosquito and can be found spreading the virus in the outdoors. DOH is however unsure if this specie of Aedes mosquito is the one responsible for the cases of dengue nowadays.
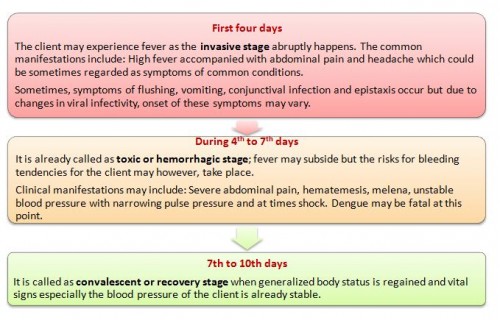
The etiologic agents carried by the vector mosquito include Dengue Virus Types 1, 2, 3, 4, and Chikungunya virus. The condition causes an acute febrile infection with sudden onset that could be manifested in three stages:
- Incubation Period: Approximately one week
- Period of Communicability: Upon infection of virus in the blood, within the first week of illness.
- Susceptibility, Resistance, and Occurrence: It is universal with both sexes equally affected. It primarily involves children aging 5- 9 years, especially those in preschool and school ages. However, it does not exempt adults and infants. It is an acquired illness through the said vector with temporary immunity, though to some cases it is permanent.
It is sporadic throughout the year according to statistics and becomes epidemic during the months of June to November.
Classification of Dengue Hemorrhagic Fever: (Depending on Severity)
- Mild – Client may manifest fever, with or without petechial hemorrhage.
- Moderate – Client may experience high fever, but with less hemorrhage and no progression to shock.
- Severe, frank type- Sudden onset of fever may occur with severe hemorrhage; which is accompanied by an abrupt decrease in temperature, shock and termination of recovery.
Grading of Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS) According to 2010 Guideline:
- DHF Grade I: Fever accompanied by non- specific symptoms like anorexia, vomiting, and abdominal pain; the only hemorrhagic manifestation is (+) tourniquet test and/ or easy bruising
- DHF Grade II: Spontaneous bleeding plus the manifestations with Grade I (usually observed in GIT or mucocutaneous
- DHF Grade III (DSS): Presence of circulatory failure as evidenced by rapid, weak pulse, narrowing of pulse pressure or hypotension, and cold clammy skin.
- DHF Grade IV (DSS): Profound shock with undetectable blood pressure or pulse.
Dengue Hemorrhagic Fever Nursing Considerations and Care Management
- Preventive and control measures that would involve health education and strongly advocating the implementation of 4S, recognition of the disease, case finding, and reporting for cases in the community.
The Four S drive implemented by the Department of Health corresponds to:
- Search and destroy the mosquito dengue carrier’s breeding sites (recently pinpointing buko shell or coconut shells, tires, and bromeliads)
It may also involve frequent changing of water and scrubbing sides of vases and keeping water containers covered at all times, destroying of breeding places stated above by cleaning the surroundings (3 O’clock habit) and proper disposal of tires and containers.
- Self-protection against mosquito (use of loose clothing with long sleeves and long socks, use of mosquito nets, tested mosquito repellants and the like)
- Seek early consultation (Early detection of the condition means the treatment could be administered readily to prevent fatal complications of dengue)
- Say NO to indiscriminate fogging (Fogging is not advised nowadays because it does not really eliminate mosquitoes but it only scares them away. It is also not recommended because of its respiratory consequences.)
Supportive management which could be symptomatic in nature may involve:
- Rapid replacement of fluids: clients are encouraged to increase their fluid intakes as much as possible if tolerated; In the community, ORS is given to halt moderate dehydration at 75ml/ kg in 4 -6 hours or up to 2- 3 liters in adults.
- Administration of antipyretic/ analgesics as indicated by the physician
- Close observation and intensive monitoring of vital signs
- Early detection for signs of bleeding and immediate referral
- Use of Tourniquet test (Rumpel Leade test) to detect petechial hemorrhage
Health education on the prevention of hemorrhage may include:
- Avoidance of dark-colored foods and liquids
- The client is encouraged to prevent from using sharp- bristled toothbrushes, instead advised to gargle with saline solution
- Clients are educated not to use hot liquids for the alleviation of chills etc.
- Avoidance of sharp objects like razors are emphasized on adults
- The use of ASPIRIN is strictly prohibited.
In cases that hemorrhage sets in, nursing care may involve the following:
- Keep the client at bed rest and ensure safety to prevent from injury
- The client is usually placed in dorsal recumbent position.
- Hourly monitoring noting for narrowing pulse pressure, a sudden drop in temperature, decreased blood pressure and pulse rate, and other signs of deterioration.
- Administration of blood products and monitoring clients for signs of adverse reactions.
- Strict monitoring of fluid intake and output
- Immediate referral for any change in the client’s status and proper documentation of procedures given.
References
- Center for Disease Control and Prevention. (May 16, 2012). Update: Dengue in Tropical and Subtropical Regions. Retrieved last May 23, 2012 from http://wwwnc.cdc.gov/travel/notices/in-the-news/dengue-tropical-sub tropical.htmGonzales, M.L.A., et.al. (October 2010).
- 2010 Interim Guidelines on Fluid Management of DF/DHF. Retrieved last May 24, 2012 from http://ppsstc.com/files/2010%20PPS%20Guidelines%20on%20Dengue.pdfPhilippine Nurse’s Association. (May 17, 2012). DOH Targets No More Than 100, 000 Dengue Cases for 2012. Retrieved last May 20, 2012 from http://www.pna.gov.ph/index.php?idn=&nid=7&rid=426651Philippine Nurse’s Association. (May 16,
- 2012). DOH Urges Public to Continue Search and Destroy of Dengue Mosquito Breeding Sites. Retrieved last May 20, 2012 from http://www.pna.gov.ph/index.php?idn=&nid=7&rid=426358 Reyala, J.P., et.al.
- (2000).Community Health Nursing Services in the Philippine Department of Health. 9th Edition.









Grateful thanks, but I wanna receive pathophysiology of DHF.
thanks carol…=)