Have you collected cola-colored urine from a patient diagnosed with acute glomerulonephritis and wondered how it formed? This article explains AGN to enhance your understanding.
Acute glomerulonephritis (AGN) is a serious kidney condition with significant patient implications. Understanding AGN is crucial for nurses and student nurses, as they play a vital role in identifying early signs such as hematuria, proteinuria, and hypertension. Early detection can lead to timely medical intervention and help prevent complications like acute kidney injury, heart failure, and pulmonary edema. Nurses with knowledge of AGN can provide better care through proper treatment, dietary education, and fluid management.
Anatomy and Physiology of the Kidneys
The kidneys, located below the rib cage on either side of the spine, maintain the body’s balance of fluids, electrolytes, and waste products.
Anatomy (Microanatomy)
- Nephrons: Functional units of the kidneys.
- Glomerulus: Capillary network in each nephron that filters blood.
- Renal Tubules: Transport filtered fluid through the kidney.
- Collecting Ducts: Carry filtrate from nephrons to the ureters.
Functions
- Filtration: Removes waste products like urea and creatinine from the blood.
- Reabsorption: Returns essential substances like glucose and electrolytes to the bloodstream.
- Secretion: Eliminates waste products and maintains blood pH.
- Hormone Production: Produces erythropoietin (stimulates red blood cell production) and renin (regulates blood pressure).
What is Acute Glomerulonephritis?
AGN is a sudden kidney disorder characterized by inflammation of the glomeruli, the kidney’s filtering units. It can arise from infections or autoimmune diseases. Nurses need to understand the causes, pathophysiology, diagnostic process, treatment, and interventions to manage AGN effectively.
Causes of Acute Glomerulonephritis
- Infections: Post-streptococcal glomerulonephritis, after strep throat or skin infections, is the most common cause. Other viral infections like hepatitis and HIV can also lead to AGN.
- Autoimmune Diseases: Conditions such as lupus or IgA nephropathy cause immune-mediated glomerular damage.
- Other Factors: Medications, toxins, and systemic diseases like Henoch-Schönlein purpura.
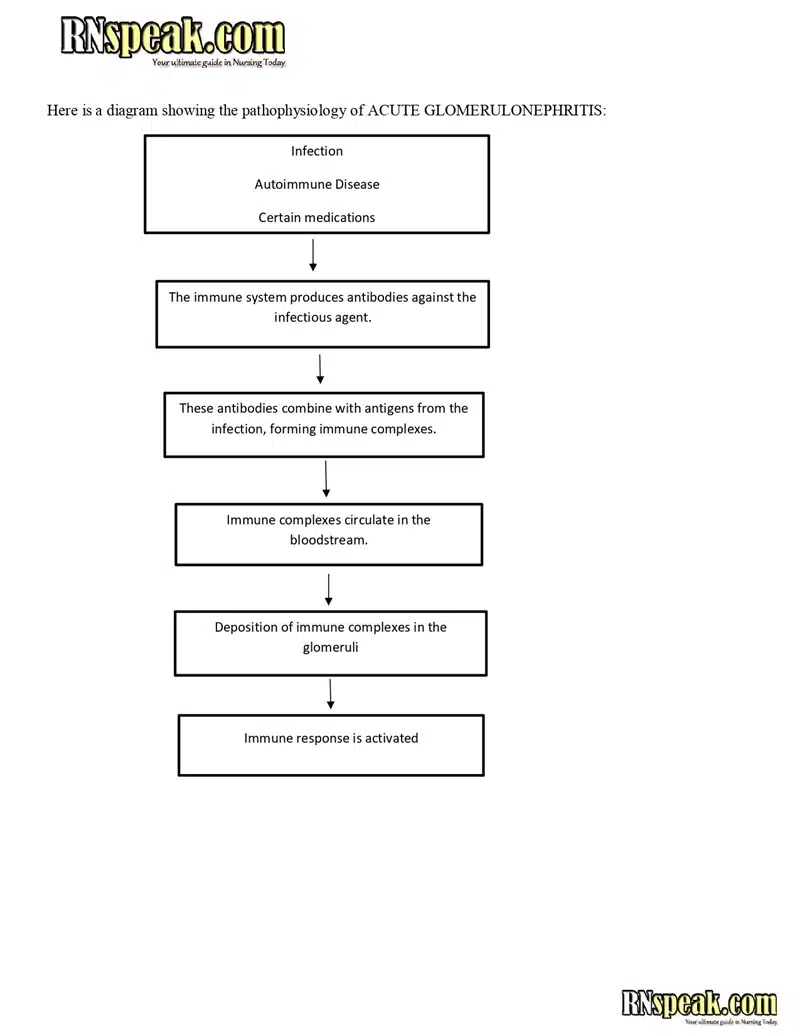
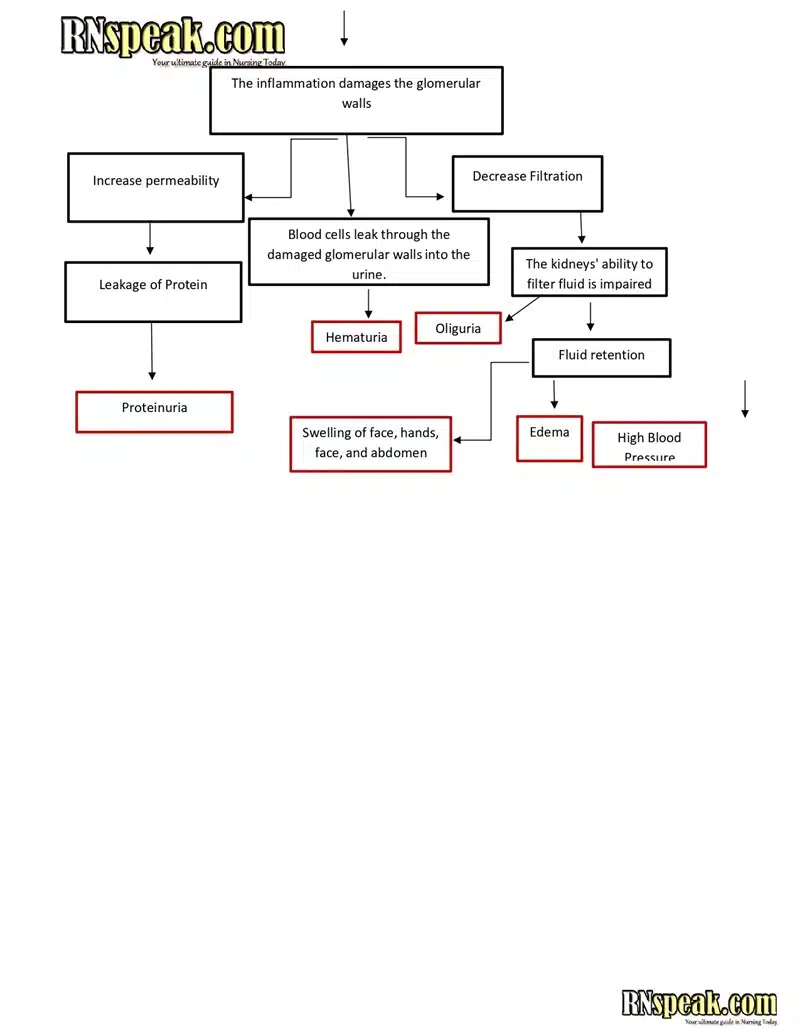
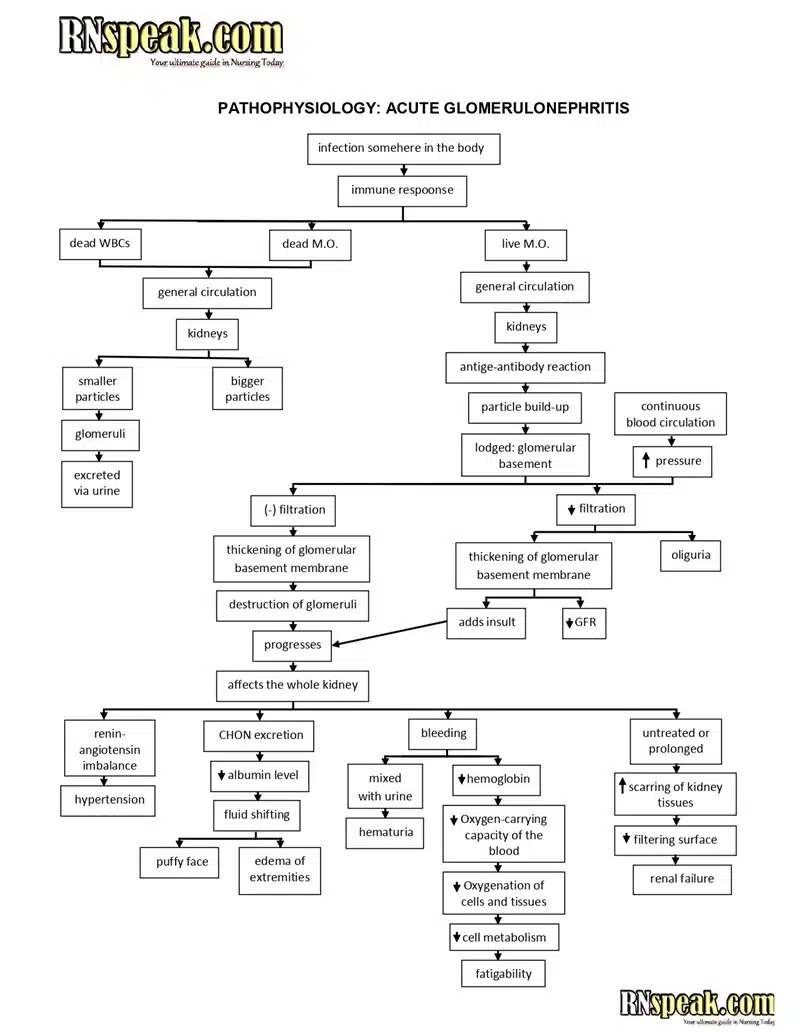
Pathophysiology
In AGN, inflamed glomeruli become more permeable, leading to the leakage of blood cells and proteins into the urine (hematuria and proteinuria). Reduced glomerular filtration rate (GFR) leads to fluid retention, hypertension, and edema. If untreated, AGN can progress to chronic kidney disease or failure.
Acute Glomerulonephritis (AGN) Pathophysiology & Schematic Diagram
Acute Glomerulonephritis (AGN) Schematic Diagram 2
Clinical Manifestations
- Urinary Changes: Hematuria (cola-colored urine), proteinuria (foamy urine), oliguria (decreased urine output).
- Systemic Symptoms: Edema, hypertension, fatigue, fever, nausea, vomiting.
Diagnostic Procedures
- Medical History and Physical Exam: Detects symptoms like fatigue, hypertension, and swelling.
- Urinalysis: Checks for red blood cells, white blood cells, and protein in the urine.
- Blood Tests: Evaluate kidney function by measuring creatinine and blood urea nitrogen (BUN) levels.
- Imaging Studies: Ultrasound assesses kidney size and structure; biopsy may determine the type of glomerulonephritis.
Treatment
Treatment depends on the cause and severity of AGN:
- Medications: Corticosteroids reduce inflammation; ACE inhibitors control blood pressure and protect kidney function.
- Dietary Modifications: Restrict salt and protein to reduce kidney workload and manage fluid retention.
- Management of Underlying Conditions: Antibiotics may treat infections, and immunosuppressants may be necessary for autoimmune causes.
- Advanced Cases: Dialysis or kidney transplantation may be required for severe kidney damage.
Nursing Interventions
- Monitor Vital Signs: Regularly check blood pressure and heart rate due to hypertension risk.
- Fluid Management: Track intake and output to prevent complications like pulmonary edema.
- Patient Education: Teach patients about dietary restrictions, medication adherence, and recognizing worsening symptoms.
- Provide Psychological Support: Offer emotional support to patients and families.
- Collaborate with Healthcare Providers: Ensure comprehensive care, including specialist referrals.
Conclusion
Acute glomerulonephritis is a serious condition requiring timely diagnosis and treatment. Understanding its causes, pathophysiology, and management strategies is essential for nurses to provide effective care and improve patient outcomes.