Have you encountered a patient experiencing pain in the upper abdomen radiating to the back? This symptom might lead to different diagnoses, but we, as nurses, need to determine if it is pancreatitis or not. Pancreatitis is a potentially life-threatening condition that requires comprehensive nursing care. Understanding the pathophysiology and management of pancreatitis is important to be able to provide effective management strategies and timely nursing interventions.

One study shows that there has been an increase in the global incidence of acute pancreatitis, most especially in Western countries (Kaplan et al., 2021). Men and women are equally susceptible to acute pancreatitis, even though the causes of pancreatitis vary depending on gender.
Pancreatitis is simply defined as inflammation of the pancreas, which can be acute or chronic. It is a result of autodigestion by the pancreatic enzymes caused by obstruction of pancreatic ducts (e.g., edema, tumor, inflammation, and gallstones) and other causes.
Anatomy and Physiology
The pancreas is a gland located behind the stomach and adjacent to the small intestine. This gland is responsible for producing enzymes that play a vital role in digestion and hormones that help regulate blood sugar levels. The pancreas has both endocrine and exocrine functions.
Endocrine Function
The pancreatic islets, also known as the islets of Langerhans, produce:
- Alpha Cells (glucagon) – Stimulate the liver to break down stored glycogen into glucose (hyperglycemic agent).
- Beta Cells (insulin) – Lower blood sugar levels (hypoglycemic agent).
- Somatostatin – Regulates the secretion of glucagon and insulin.
Exocrine Function
The pancreas also produces “pancreatic juice,” which is essential for breaking down food in the small intestine. This enzyme-rich juice contains:
- Amylase – Responsible for the digestion of starch or carbohydrates.
- Lipase – Responsible for the digestion of fats.
- Trypsin, chymotrypsin, and others – Responsible for the digestion of proteins. Trypsin is also the enzyme that can cause autodigestion.
Let us explore more about pancreatitis and its management in the following sections.
Clinical Manifestations
Symptoms of pancreatitis range from mild to severe, depending on the extent of the inflammation and whether it is acute (lasting a few days) or chronic (lasting longer periods). The main symptoms observed in a patient diagnosed with pancreatitis include:
- Severe abdominal pain: The most common symptom, often described as a constant or intermittent sharp or dull sensation that can radiate to the back or below the left shoulder blade.
- Nausea and vomiting: Patients may experience nausea and vomiting due to irritation in the lining of the stomach and intestine when the pancreas becomes inflamed. This can lead to dehydration and electrolyte imbalances.
- Abdominal tenderness and guarding: The abdomen may be tender upon palpation, and the patient may exhibit guarding in the upper abdomen as a protective response to pain.
- Abdominal distension: The abdomen may become swollen due to the accumulation of fluid and gas. Inflammation disrupts normal digestion, leading to increased intra-abdominal pressure and distension.
- Fever: Patients may develop a fever as a result of the inflammatory response and infection.
- Jaundice: In cases of obstructive pancreatitis, patients may exhibit yellowing of the skin and eyes due to the blockage of bile ducts, a condition known as jaundice.
Type of Pancreatitis
There are two types of pancreatitis, depending on the severity and duration of the condition:
Acute Pancreatitis
This type of pancreatitis is temporary and occurs when the pancreas becomes inflamed due to minor injuries or trauma. It usually lasts for a few days and can be treated with supportive care, such as rest, hydration, and pain relievers.
Chronic Pancreatitis
This condition is long-term and progressive, where the pancreas becomes chronically inflamed. It can cause permanent damage to the pancreas, leading to scarring, loss of function, and chronic pain.
Causes
Inflammation of the pancreas can be caused by several factors, including:
- Gallstones: Gallstones block the pancreatic duct, leading to acute pancreatitis. These small stones form in the gallbladder and can sometimes pass into the bile duct, blocking the pancreas and causing inflammation.
- Excessive alcohol consumption: Drinking excessive amounts of alcohol can lead to pancreatitis due to the toxic byproducts of alcohol in the blood.
- Hypertriglyceridemia: High levels of triglycerides in the blood can cause pancreatitis. This condition is often associated with obesity and other metabolic disorders. High concentrations of triglycerides can lead to the formation of free fatty acids through the action of pancreatic lipase, causing pancreatic cytotoxicity and local injury, resulting in inflammation and pancreatitis.
- Genetic disorders: Certain genetic conditions, such as cystic fibrosis, can increase the risk of developing chronic pancreatitis. This increased risk is due to genetic defects in the CFTR gene, leading to pancreatic duct obstruction and inflammation.
- Other medical conditions: Conditions such as autoimmune diseases, infections, and metabolic disorders can also cause chronic pancreatitis.
Risks and Complications
If not treated immediately, pancreatitis can lead to several complications, including:
- Infection: Patients with pancreatitis are at risk of developing infections, particularly in the lungs and bloodstream. The severe inflammatory response can translocate the infection from the gut to the bloodstream.
- Pseudocysts: Pseudocysts are collections of fluid, enzymes, and debris that form in or around the pancreas following pancreatitis. They develop because the ducts within the pancreas can become blocked or damaged during inflammation. These cysts can grow, causing pain, obstructing surrounding organs, or becoming infected. If a pseudocyst ruptures, it can lead to internal bleeding or peritonitis, a severe infection of the abdominal cavity.
- Diabetes: Developing diabetes mellitus is common following acute pancreatitis, likely due to damage to the pancreas. The pancreas produces insulin, which regulates blood sugar levels. Pancreatitis can damage the insulin-producing beta cells, leading to insufficient insulin production and the development of diabetes mellitus.
- Malnutrition: Patients with chronic pancreatitis may experience malnutrition due to impaired pancreatic secretions and increased nutritional needs. The pancreas secretes enzymes essential for digesting carbohydrates, proteins, and fats. Without adequate enzyme production, patients cannot properly digest food, leading to nutrient deficiencies, weight loss, and malnutrition. Additionally, increased metabolic demands from chronic inflammation further exacerbate nutritional deficiencies.
Diagnostic Tests
Determining the presence of pancreatitis involves a two-step approach. First, the doctor will gather information about the patient’s medical history and symptoms. Second, tests and procedures will be recommended to confirm the diagnosis.
- Physical examination: The doctor will press on the abdomen to check for tenderness and swelling. They might also listen for abnormal bowel sounds.
- Blood tests: Blood tests are usually the first line of defense to diagnose pancreatitis. These tests measure the levels of digestive enzymes, amylase, and lipase produced by the pancreas. In the case of pancreatitis, the levels of these enzymes in the blood increase.
- Stool tests: A stool test might be recommended to check for fat malabsorption, a potential sign of pancreatic insufficiency. Normally, the digestive enzymes produced by the pancreas help break down fats. If the pancreas is not functioning properly, undigested fat will be detected in the stool.
- Imaging tests:
- Ultrasound: This painless imaging test uses sound waves to create a picture of the pancreas, gallbladder, and bile ducts. It can help detect gallstones, a common cause of pancreatitis.
- CT scan: A CT scan uses X-rays to create detailed cross-sectional images of the abdomen. It can provide a clearer picture of the pancreas, including the extent of inflammation and any blockages in the pancreatic duct or bile duct.
- MRI scan: Magnetic resonance imaging (MRI) uses strong magnetic fields and radio waves to produce detailed images of abdominal organs. It can be especially useful if a CT scan is inconclusive or if the doctor suspects other causes of abdominal pain.
- Endoscopic ultrasound (EUS): This procedure involves inserting a thin, flexible tube with a tiny ultrasound device at its tip through the mouth and into the upper digestive tract. EUS provides a detailed view of the pancreas and surrounding structures, including any tumors or blockages.
- Pancreatic function test (PFT): This test measures how well the pancreas is digesting and absorbing nutrients. It usually involves ingesting a liquid containing a special sugar and then collecting stool samples over the next few hours. The amount of sugar in the stool helps determine how well the pancreas is functioning.
It’s important to remember that these tests are used together to diagnose pancreatitis. No single test is definitive.
Treatment and Management
The treatment for pancreatitis involves managing symptoms, addressing underlying causes, and preventing complications. This includes:
- Pain management: Patients are typically given pain medications, such as parenteral opioids, to manage their discomfort.
- Fluid and electrolyte management: Intravenous fluids are administered to manage dehydration and electrolyte imbalances.
- Nutritional support: Patients are often given a diet high in carbohydrates and low in fats and proteins to help manage their nutritional needs.
- Pancreatic enzyme replacement: Patients with chronic pancreatitis may require pancreatic enzyme supplements to aid in digestion.
- Counseling and education: Patients are educated on lifestyle changes, such as avoiding high-fat foods, heavy meals, and alcohol, to prevent future episodes.
Nursing interventions for patients with pancreatitis focus on managing symptoms, preventing complications, and promoting recovery. These interventions include:
- Pain management: Assess and manage pain associated with pancreatitis using pharmacological and non-pharmacological methods. Post-surgical care includes administering pain relievers as prescribed.
- Fluid and electrolyte management: Monitor and manage fluid and electrolyte levels to prevent dehydration and Replace electrolytes such as sodium, potassium, and chloride to maintain proper balance. Vital signs should be closely monitored, including blood pressure, pulse, and temperature, to detect any signs of dehydration or electrolyte imbalance.
- Nutritional support: Educate patients on dietary modifications and provide nutritional support as needed. Teach patients about dietary restrictions, such as avoiding fatty or spicy foods, to reduce inflammation and promote healing. Provide nutritional supplements, such as pancreatic enzymes, to support digestion and absorption. Administer enteral nutrition, such as tube feeding, to ensure adequate nutrition when oral intake is impossible.
- Infection prevention: Take measures to prevent infections, such as maintaining proper hygiene and administering antibiotics as prescribed. Provide aseptic wound cleaning to prevent further infection if there is a surgical wound.
- Patient education: Teach patients about the risks and complications of pancreatitis and lifestyle changes to prevent future episodes.
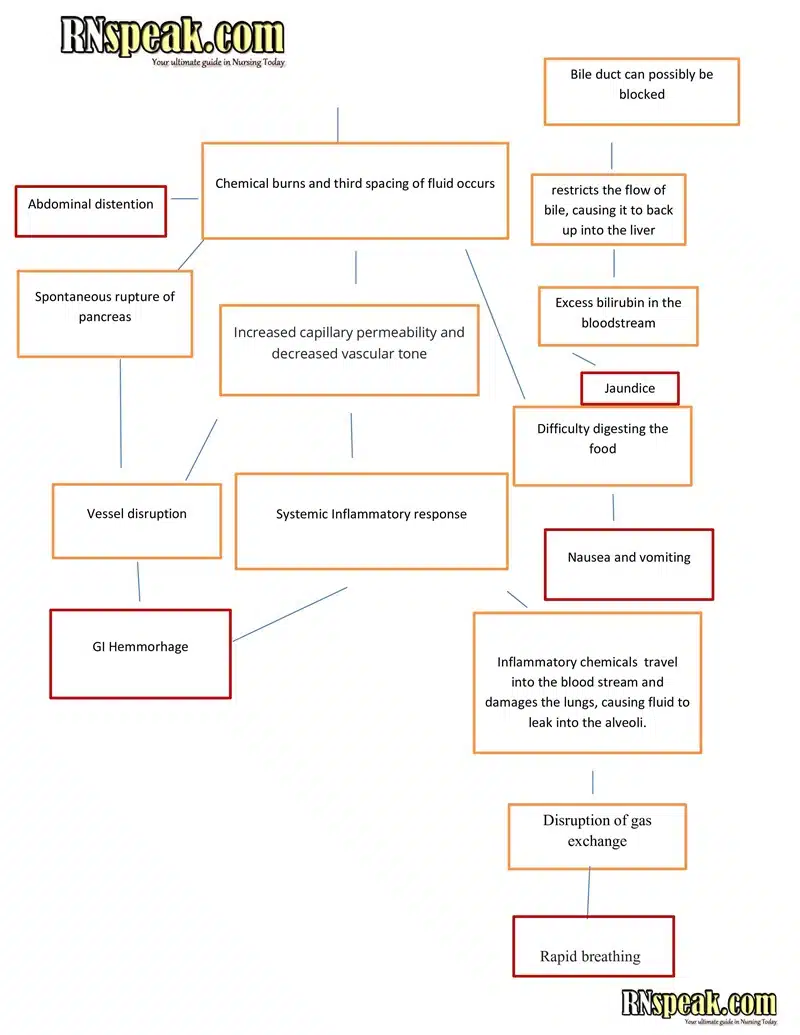
Acute Pancreatitis Pathophysiology in Schematic Diagram
Conclusion
Pancreatitis is a severe condition that requires immediate medical attention. Understanding the clinical signs, risks, and treatment options is essential to provide effective management and prevent complications. Providing appropriate care to patients with pancreatitis involves concentrating on symptom management, preventing complications, and facilitating recovery through health education and lifestyle changes.
References
- Hinkle, J. L., & Cheever, K. H. (2014). Brunner & Suddarth’s textbook of medical-surgical nursing (Edition 13.). Wolters Kluwer Health/Lippincott Williams & Wilkins.
- Bartel, M. (n.d.). Acute Pancreatitis. Retrieved June 14, 2024, from MSD Manual Professional Edition website: https://www.msdmanuals.com/professional/gastrointestinal-disorders/pancreatitis/acute-pancreatitis
- Iannuzzi, J. P., King, J. A., Leong, J. H., Quan, J., Windsor, J. W., Tanyingoh, D., … Kaplan, G. G. (2022). Global incidence of acute pancreatitis is increasing over time: A systematic review and meta-analysis. Gastroenterology, 162(1), 122–134. doi:10.1053/j.gastro.2021.09.043