Congestive heart failure (CHF) continues to be a leading global health issue, affecting over 64 million people worldwide (Shahim et. al, 2023) and contributing significantly to hospitalizations and healthcare costs (World Heart Federation, 2023). In the United States alone, nearly 6.7 million adults live with CHF (CDC, 2024), while its prevalence continues to rise in aging populations and regions with limited access to healthcare. This chronic condition, which is characterized by the heart’s inability to pump blood effectively, results in symptoms such as fatigue, shortness of breath, and fluid retention. Despite advancements in treatment, CHF remains a leading cause of mortality.
Understanding the pathophysiology of CHF is crucial for improving patient care and outcomes. CHF isn’t just a cardiac issue—it involves complex interactions between the heart, kidneys, and other body systems, creating a vicious cycle of worsening symptoms. With a strong grasp of this knowledge, it becomes easier to anticipate complications, educate patients on prevention and symptom management, and implement evidence-based interventions to slow disease progression. As frontline healthcare providers, nurses play a vital role in improving the quality of life for those living with this challenging condition.
What is Congestive Heart Failure?
Congestive heart failure (CHF), otherwise known as cardiac failure, refers to the inability of the heart to pump sufficient blood to meet the needs of tissues for oxygenation and nutrition. This disease can affect the heart’s ability to respond to the circulation demands of the body. CHF is a slowly developing condition where cardiac output is lower than normal.
Congestive heart failure (CHF) can be classified based on which side of the heart is primarily affected. Traditionally, heart failure is divided into left-sided heart failure and right-sided heart failure. However, it’s essential to note that the heart functions as an integrated pump, and changes in one chamber can affect the entire heart.
Left-sided heart failure typically involves the left ventricle, which is responsible for pumping oxygenated blood to the body. This type of failure often results from conditions like hypertension, coronary artery disease, or cardiomyopathy. Symptoms may include shortness of breath (dyspnea), fatigue, and swelling in the legs and feet due to fluid buildup. Right-sided heart failure affects the right ventricle, which pumps blood to the lungs. It can be caused by conditions such as pulmonary hypertension or heart valve problems. Symptoms may include swelling in the legs and abdomen (ascites) due to fluid accumulation.
In practice, distinguishing between left and right heart failure is somewhat misleading because both sides of the heart are interconnected. However, this classification helps guide initial evaluations and treatments. Left-sided failure requires different management strategies compared to right-sided failure. In addition, heart failure can also be classified based on the ejection fraction (EF), into heart failure with reduced ejection fraction (HFrEF) and heart failure with preserved ejection fraction (HFpEF), which further influences treatment approaches.
Signs and Symptoms
Congestive heart failure (CHF) is characterized by a range of symptoms that can vary depending on the severity and progression of the condition. Common signs include:
- Shortness of Breath
This is often one of the earliest symptoms, occurring during physical activity or even at rest. It can worsen when lying down, leading to nocturnal awakenings due to difficulty breathing.
- Fatigue and Weakness
Even after rest, extreme tiredness is a trademark symptom, making daily activities challenging. This is due to the heart’s inability to pump enough oxygen-rich blood to meet the body’s needs.
- Edema (especially in lower extremities)
Fluid retention causes swelling in the ankles, legs, and feet. Fluid can also accumulate in the abdomen, leading to bloating.
- Coughing
A persistent cough, sometimes worse at night, may occur due to fluid accumulation in the lungs.
- Palpitations
Rapid or irregular heartbeats, known as palpitations, occur because the heart is working harder to pump blood.
- Gastrointestinal Symptoms
Loss of appetite, nausea, and abdominal swelling are common in CHF because it causes the blood and fluid to back up in the digestive system, leading to congestion.
- Neurological Symptoms
Confusion and decreased alertness may occur due to reduced blood flow to the brain.
Diagnostic Tests
Diagnosing congestive heart failure (CHF) involves several tests to assess the heart’s function and identify any underlying causes. Here are the common diagnostic tests:
- Medical History and Physical Examination. The medical history helps identify symptoms, past illnesses, and lifestyle factors that could contribute to CHF, including questions about shortness of breath, fatigue, and swelling, as well as past conditions like hypertension or heart disease. The physical examination assesses the patient’s condition for signs of heart failure, including vital signs, heart sounds, signs of fluid accumulation in the lungs, abdominal swelling, and peripheral edema.
- Blood Tests. Blood tests can reveal the presence of proteins like B-type natriuretic peptide (BNP) that indicate heart stress. They also help identify other conditions that might be contributing to symptoms.
- Electrocardiogram (ECG or EKG). This test records the heart’s electrical activity to detect irregular heartbeats or other issues.
- Echocardiogram. This diagnostic procedure uses sound waves to create images of the heart, showing how well it pumps blood and if there are any valve problems.
- Chest X-ray. Chest X-ray helps determine if the heart is enlarged or if there is fluid in the lungs, which can be signs of CHF.
- Breathing Tests. These assess lung function and check for conditions that might be causing breathing difficulties.
- Exercise Stress Test. Exercise stress tests measure how the heart responds to physical activity, which can reveal symptoms of heart failure during exercise.
- Advanced Imaging Tests. Imaging tests such as CT scans, MRI scans, or nuclear heart scans can provide detailed images of the heart’s structure and function.
Treatment and Management
The treatment and management of congestive heart failure (CHF) require a multifaceted approach that includes lifestyle changes, medications, and sometimes surgical interventions. Lifestyle adjustments are essential, such as following a low-sodium diet to reduce fluid retention, limiting caffeine and alcohol intake, maintaining a healthy weight, quitting smoking, and engaging in regular physical activity like walking or participating in cardiac rehabilitation programs.
Medications play a key role, with ACE inhibitors and ARBs relaxing blood vessels, beta blockers reducing heart rate and workload, diuretics helping manage fluid buildup, aldosterone antagonists assisting with fluid retention, and vasodilators widening blood vessels to lower blood pressure.
Surgical options may include coronary artery bypass grafting, heart valve repair or replacement, implantable cardioverter defibrillators to help prevent dangerous heart rhythms, cardiac resynchronization therapy to improve heart function, ventricular assist devices to support the heart, and in severe cases, a heart transplant. Regular monitoring and follow-up care are essential for effective management, along with addressing related conditions like sleep apnea.
Pathophysiology
In CHF, the contractile properties of the heart are impaired. This leads to a decreased cardiac output. Cardiac output (CO) is best described by the equation CO = HR (heart rate) x SV (stroke volume). Heart rate is an autonomic nervous system function, and in cases where CO falls, the sympathetic nervous system increases heart rate to maintain adequate cardiac output. When the compensatory mechanism fails to maintain adequate tissue perfusion, the properties of stroke volume must adjust to maintain CO. However, if the main problem in CHF is the damage of heart muscle fibers, stroke volume is impaired, and CO cannot be maintained to normal output.
The amount of blood pumped in each contraction is what you call the stroke volume (SV). SV is dependent on three factors, namely the preload, which is the volume of blood filling the heart. The amount of blood brought to the heart is directly proportional to the pressure applied by the length of the stretch of the myocardial fibers. The second factor relating to stroke volume is the changes in the force of contraction occurring at the cellular level, which is termed contractility. This factor is related to the length of myocardial fibers and the levels of calcium in the body. The third factor is referred to as afterload. This is the amount of pressure of ventricles need to come up to be able to pump blood across the pressure gradient that is created with the arteriole resistance.
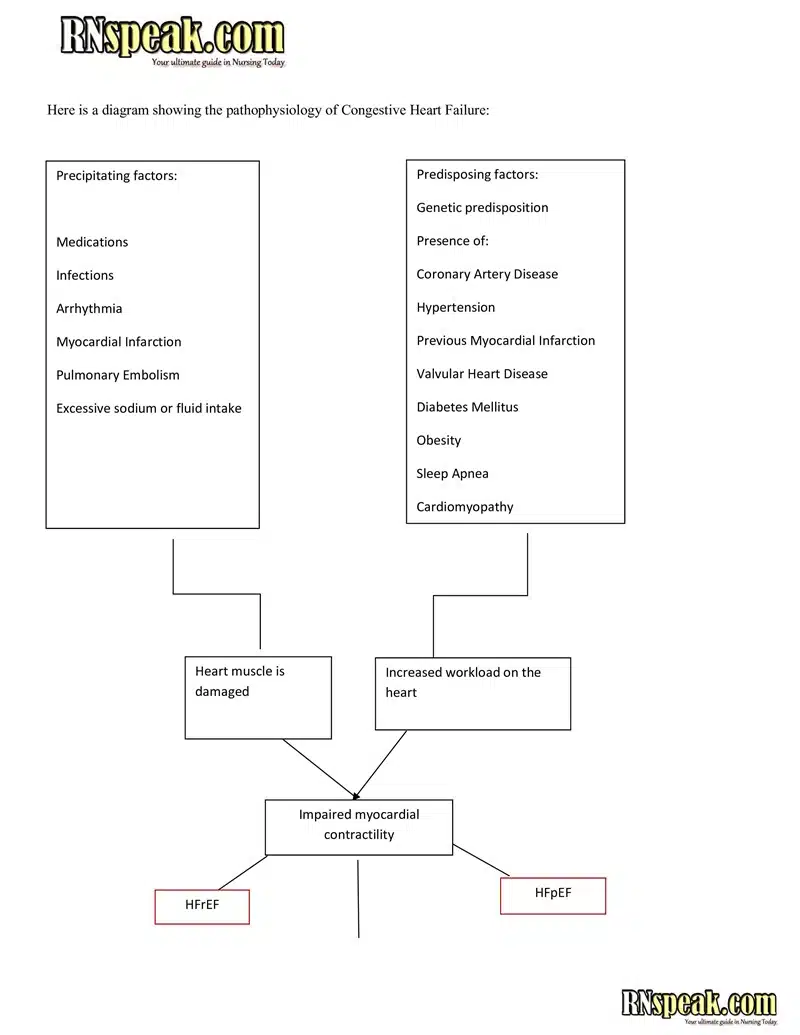
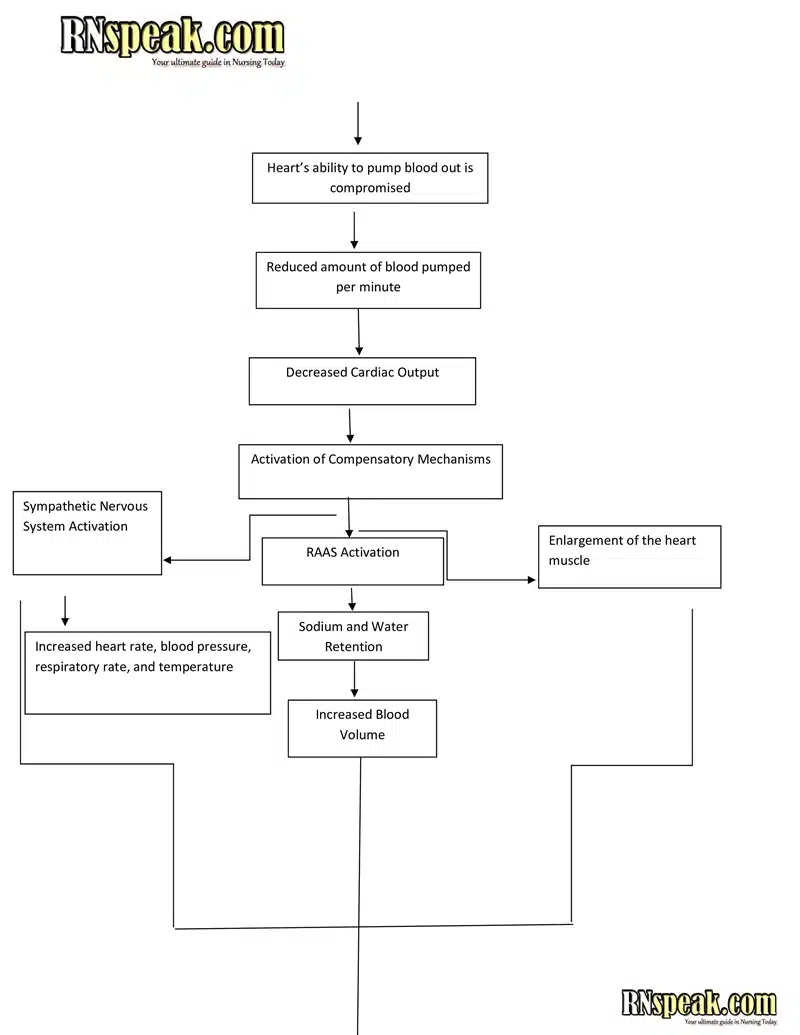
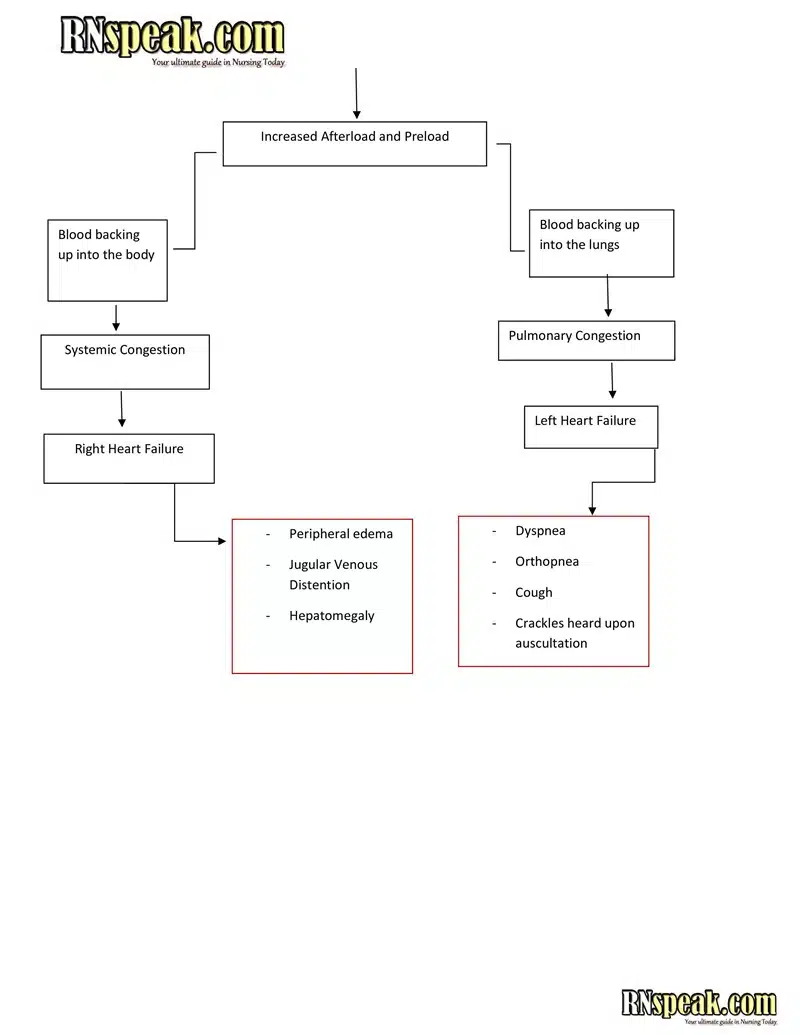
Congestive Heart Failure Pathophysiology Schematic Diagram
Etiology of CHF
The following are the common etiologies of Congestive Heart Failure:
Myocardial Weakness
Myocardial weakness often results from ischemia due to atherosclerosis and stenosis of the coronary arteries. When stenosis reaches about 70-90%, the heart’s demand for oxygen during stress cannot be met, and even resting myocardial oxygen supply may be compromised at higher levels of blockage. As atherosclerosis progresses, myocardial fibers undergo hypoxic injury, leading to necrosis. These fibers are then replaced with fibrous connective tissue, resulting in the deteriorating pumping capacity of the heart and reduced ventricular compliance. Other causes of myocardial ischemia include thrombosis in the coronary arteries. Myocardial weakness can develop with myocarditis or cardiomyopathies.
Restrictions to Pumping
Several physical factors can restrict the heart’s pumping ability:
- Malfunctioning cardiac valves: The Inability of the valves to open widely (stenosis) or close properly (regurgitation) can decrease blood flow, leading to reduced cardiac output.
- Congenital Heart Defects: These defects can interfere with the free flow of blood, affecting the heart’s pumping efficiency.
- Presence of masses: Tumors or thrombi within cardiac chambers can cause internal obstruction by occupying part of the chamber’s volume, thereby reducing its blood capacity. The most common cardiac tumor, myxoma, is of endothelial origin and is often located in the left atrium, accounting for about 50% of primary cardiac tumors. Its presence can occlude the mitral valve or serve as a site for thromboembolus formation.
- Cardiac dysrhythmias, pericarditis, and cardiac tamponade can also restrict pumping by disrupting normal heart function.
Increased Afterload
Inability to maintain cardiac output may also result from increased afterload. When the myocardium is constantly exposed to high physical demand, the strain can overwhelm the heart, leading to declined contractility and stroke volume. This is often seen when cardiac afterload is increased in the following conditions:
- Cor Pulmonale. Right ventricular overload due to lung diseases causing pulmonary hypertension can increase afterload on the right ventricle.
- Systemic hypertension. Elevated blood pressure presents an increased resistance that the left ventricle must overcome to maintain adequate cardiac output.
- Valve disease or congenital defects in the cardiac outflow tracts, valves, pulmonary trunk, or aorta can also produce excessive ventricular afterload.
Conclusion
Congestive Heart Failure is a complex condition that requires a thorough understanding for effective management. Recognizing the disease process is essential in improving patient outcomes. Identifying signs and symptoms, understanding the underlying pathophysiology, and being well-versed in appropriate diagnostic procedures and treatment strategies enable the delivery of compassionate, evidence-based care. Additionally, educating patients, supporting lifestyle modifications, and continuously monitoring their condition play a critical role in enhancing their overall quality of life.
References
- Deaths from cardiovascular disease surged 60% globally over the last 30 years: Report. (2023, May 20). World Heart Federation. Retrieved from https://world-heart-federation.org/news/deaths-from-cardiovascular-disease-surged-60-globally-over-the-last-30-years-report/
- Shahim, B., Kapelios, C. J., Savarese, G., & Lund, L. H. (2023). Global Public Health Burden of Heart Failure: An Updated Review. Cardiac failure review, 9, e11. Retrieved from https://doi.org/10.15420/cfr.2023.05
- CDC. (2025, February 14). About heart failure. Heart Disease. https://www.cdc.gov/heart-disease/about/heart-failure.html
- King, M., Kingery, J., & Casey, B. R. (2012). Diagnosis and evaluation of heart failure. American Family Physician, 85(12), 1161–1168. https://www.aafp.org/pubs/afp/issues/2012/0615/p1161.html
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Heart failure: Learn More – Types of heart failure. [Updated 2023 Nov 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK481485/
- Schwinger R. H. G. (2021). Pathophysiology of heart failure. Cardiovascular diagnosis and therapy, 11(1), 263–276. https://doi.org/10.21037/cdt-20-302
- Ziaeian, B., & Fonarow, G. C. (2016). Epidemiology and aetiology of heart failure. Nature reviews. Cardiology, 13(6), 368–378. https://doi.org/10.1038/nrcardio.2016.25
- Canty J. M., Jr (2022). Myocardial injury, troponin release, and cardiomyocyte death in brief ischemia, failure, and ventricular remodeling. American journal of physiology. Heart and circulatory physiology, 323(1), H1–H15. https://doi.org/10.1152/ajpheart.00093.2022
- Malik A, Chhabra L. Congestive Heart Failure. [Updated 2023 Nov 5]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430873/
- Fine, N. M. (n.d.). Cor Pulmonale. MSD Manual Professional Edition. Retrieved March 20, 2025, from https://www.msdmanuals.com/professional/cardiovascular-disorders/heart-failure/cor-pulmonale