Pharmacology is one of the most challenging topics that a nurse needs to study in preparation for an exam. Apart from the need to know the names of various medications used to treat a specific disease or condition, there is also the need to understand how to safely administer these. However, the most challenging part about the exam is calculating doses of medications needed by patients with various conditions across the lifespan.
Certifying and licensure examinations expect that the entry-level nurse to demonstrate an understanding of the basic principles of medical mathematics through:
- Calculating the right doses of medications needed to be administered to a patient;
- Ensuring that the patient receives safe and effective doses of medications every time; and
- Using sound clinical judgment to determine if the doses prescribed for the patient care within the safe levels or not.
Medication Administration and the Patients’ Rights
When administering medications to a patient, you must remember that there are rights the patient has, which must be observed. Keeping these rights in mind helps in avoiding errors in medication administration and provide the patient with a safe environment for care.
There are 10 rights of the patient receiving medications that you must observe:
1. The right drug or medication. The nurse needs to ensure that the patient receives the correct medication. To do this:
a. Check for the name of the drug and the preparation.
b. Verify the name correctly. Some drugs have similar-sounding names.
c. Do not rely only on the color of the box or bottle of the drug. These may change in time.
d. If in doubt, always verify the order with the physician or another health care team member.
2. The right patient. Ensure that the drug is given to the patient needing it.
a. Check the ID band of the patient.
b. If patient is awake and conversant, ask the patient to say his name.
c. For patients with psychiatric conditions, always check identity on the information sheet located near the foot of the bed if the patient does not have an ID band.
3. The right dose. Always ensure that the dosage required to be administered to the patient is within the safe limits. You should question any order for medication if the dosage is above or below the safe limits.
4. The right route of administration. The medication can be administered per orem, through IV infusion, or via injection (intramuscular and subcutaneous). Other routes include:
a. Rectal;
b. Intranasal;
c. Intravaginal;
d. Intraocular;
e. Otic;
f. Topical and dermal; and
g. Inhalation.
5. The right time and frequency of administration. Always check the desired time of administering drugs to prevent errors. Most common time and frequency ordered:
a. PRN- as necessary;
b. OD- once a day;
c. BID- twice a day;
d. TID- thrice a day;
e. QID- four times a day;
f. HS- at hour of sleep;
g. q4, q6, q8, q12- every 4, 6, 8 or 12 hours
6. The right documentation. Document all information about medication administration in the patients’ records. Information on any side effects and adverse reactions should be included and the physician notified if any adverse reactions occur.
7. The right assessment and patient history. Allergy information, any other drugs, and substances the patient takes and past medical history can influence the action of a drug to a patient. This information should be carefully assessed by the nurse.
8. The right approach. One of the things the nurse needs to remember is how to approach the patient when giving medications. This includes approaching the patient in a calm and professional manner, stating the name of the drug and its action. The patient has the right to refuse the medication. If the nurse explains why the drug is needed, the patient needs to sign a form indicating refusal and the nurse documents it.
9. The right evaluation. Administering correct medication involves the nurse evaluating whether the drug has achieved its desired effect. Any drug-to-drug or drug-to-food interaction should be evaluated and documented.
10. The right patient education. The nurse should provide patient information about drug-related education such as:
a. Side effects;
b. Adverse reactions and when to notify the physician;
c. Allowed and prohibited foods and activity, if any;
d. Drug-to-drug interaction; and
e. Best time to take the drug (before meals or after meals).
The Pediatric Patient Receiving Medications
Pediatric patients sometimes follow a different dosage calculation for their medication needs. This is because of differences in anatomy and physiology of a child’s body is different from an adult. The nurse must always be careful in caring for pediatric patients receiving medication and ensure that the right doses are calculated before giving any medication.
Calculating Using Body Weight
One of the most common means to calculate dosages for pediatric patients is through the use of the child’s body weight. The child’s weight in kilograms (kg) is usually the most commonly used measurement in determining how much of a certain medication is supposed to be administered.
In calculating using this method, the following rules are observed:
- Ensure that the weight of the child is expressed in the appropriate unit of measurement (pounds or kilograms).
- Identify the dosage the child needs per day or single dose.
- Calculate
Example
A child was prescribed to Ceftriaxone to treat an infection. The dosage required for him to receive 100 mg/kg of body weight a day, given in 2 separate doses. If the child weighs 56 pounds, how much drug should be administered per dose
Solution:
1. Convert pounds to kilograms
1 lb. = 0.45kg
56 lbs. = 25.40k
2. Calculate the dosage for 1 day.
100 mg per kg
100 (25.40) = 2,540 mg
3. Divide the total in 2 doses.
2,540/2= 1270 mgg
Calculating Using the Body Surface Area Method
Another formula used in calculating the doses of medications given to pediatric patients is the Body Surface Area method. In this method, the amount of medication given to the child is based on the total body surface area. This can be done using the West Nomogram, a graph that contains several scales to determine the amount of medication to use. Below is an example of it:
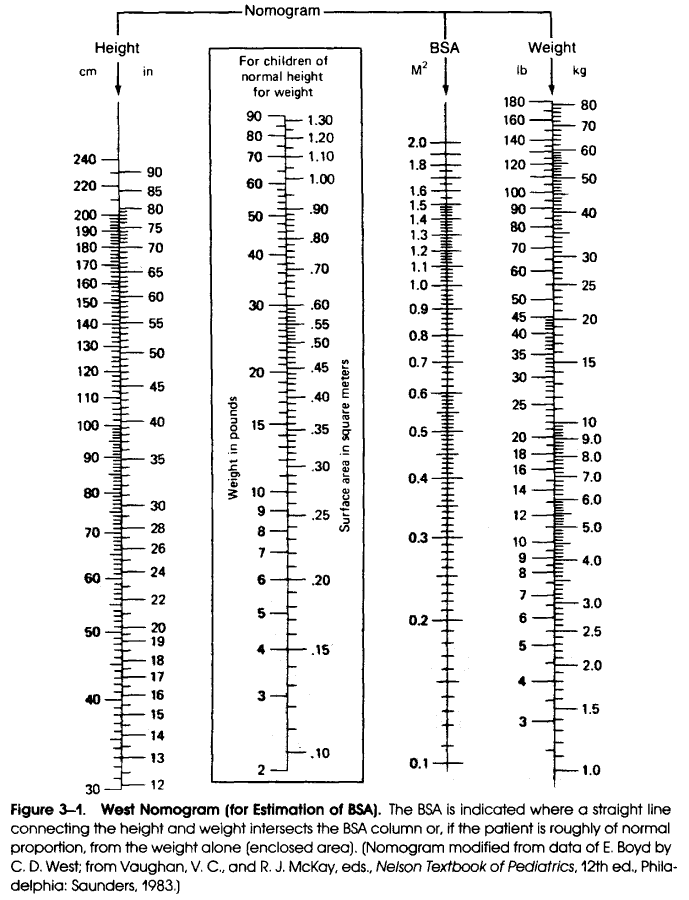
In using the West Nomogram, the nurse should remember:
- The weight of the child is usually indicated and marked on the right side of the scale. The scale can be used to signify either pounds or kilograms.
- The child’s height is located on the left side of the scale.
- It is essential to get the correct height and weight and record it on the scale. Any inaccuracies can cause under or overdosing the child.
- The two points on the left and right sides of the scales are connected using a straight line. The point where the lines meet is determined as the body surface area, expressed in square meter (m2).
- Calculate the dose using the obtained body surface area.
Example:
A child is to receive amoxicillin for an upper respiratory infection as soon as possible. However, the only available stock at the hospital pharmacy comes in adult doses of 500 mg. The nurse notifies the physician who ordered her to calculate the dosage to be given to the child using the West Nomogram. If the child’s height is 95cm and weighs 34 pounds, how much is the child to receive for his first dose?
Solution:
1. Calculate the BSA of the child using the nomogram.
*The nomogram markings will reveal the BSA of the child at 0.38m2.
2.Calculate the dosage:
Multiply stock of the drug to BSA of the child.
500 mg (0.38)
= 190 mg
Reviewing Conversion Tables
One tricky component of the dosages and calculations in nursing exams are the systems of measurements used. There are three major systems of measurements normally indicated in the dosages and calculations:
-
- Household system (more useful for health education for patients and SOs);
- Metric system; and
- Apothecary system.
The nurse needs to ensure that conversions from one system to another are made prior to calculating dosages so the risk of arriving at the wrong answers are lessened. Below are the most common conversions being used and normally asked in nurse licensure and certifying examinations.
Common Conversions
| Unit of Measurement | Equivalent |
|---|---|
| 1 teaspoon (1 tsp.) | 1 teaspoon= 6o drops 1 teaspoon= 5mL |
| 1 tablespoon (1 tbsp.) | 1 tablespoon= 3 teaspoons 1 tablespoon= 15 mL |
| 1 fluid ounce (1 fl. oz.) | 1 fl. oz.= 2 tablespoons 1 fl. oz.= 30 mL |
| 1 ounce (1 oz.); weight | 1 oz.= 30 grams 16 oz.= 1 pound |
| 1 cup | 1 cup= 8 ounces 1 cup= 16 tablespoons 1 cup= 240 mL |
| 1 pint | 1 pint= 2 cups 1 pint= 480 mL |
| 1 quart (1 qt.) | 1 quart= 2 pints 1 quart= 4 cups |
| 1 gallon (1 gal.) | 1 gallon= 4 quarts 1 gallon= 8 pints 1 gallon= 3,785 mL |
| 1 liter (1L) | 1 liter= 1,000 mL |
| 1 pound | 1 pound= 16 ounces 1 pound= 454 grams 1 pound= 0.45 kilograms |
| 1 gram (1 gr) | 1 gram = 1000 milligram (mg) 1 gram = 1,000,000 microgram (mcg) |
| 1 kilogram (kg.) | 1 kilogram= 1,000 grams 1 kilogram= 2.24pounds |
Table 1. Common Conversions (Potter, Perry and Stockhert, 2019)
Examples:
a. Convert 1.5 grams to milligrams (mg)
1.5 grams x 1,000 mg = 1,500 mg
1 gram
b. Convert 500 mL to liter
500 mL x 1 liter = 0.5L
1000 mL
c. Convert 45 mL to tablespoon
45 mL x 1 tablespoon = 3 tablespoons
15 mL
Tips in Converting
Nursing books and manuals normally use a meter, liter, and grams in expressing weight or length. Conversion is needed when these are not followed in the question stem.
- The metric system is the most widely used system of measurement.
- A household measurement system is usually used for:
- Patient health education;
- Providing patient and significant others with discharge instructions;
- Giving patient and SO a way to follow measurements using household items; and
- Enhancing compliance with dosage.
- When converting, check the units of measurement being used to see if the same measurement system is used.
- Household measurements, when converted to metric measurements are only equivalents. They are not equal.
Basic Mathematics in Dosage and Calculations
Nurse licensure exams usually ask the examinee to calculate doses of drugs and medications, IV fluids, and other therapies using whole numbers, fractions, and decimals. Below are the most common tips in overcoming these challenges:
- Whole numbers do not have decimals and fractions. They are the easiest to solve.
- Fractions in some questions may be proper fractions or improper fractions.
- Proper fractions- numerator is smaller than the denominator.
- Improper fractions- numerator is larger than the denominator; is always more than 1 when rounded to whole numbers (e.g., 5/4= 1 ¼)
- Decimals are usually rounded off to the 2nd decimal place, or the nearest hundredth. This depends on how the question is stated.
- Example:
-
- 237 is rounded off as 1.24
- 621 is rounded off as 5.62
- Rounding off decimals follow the standard mathematical rounding off rules.
-
- Ratio and proportion can be written in various ways:
-
- 1 for every 6= 1/6, 1:6 or 1 to 6
- Do not confuse ratio and proportion for fractions. Always read the entire question first and understand what is being asked.
-
Tips in Calculating Dosages Correctly
-
- Always check the calculation question and the prescription first.
- Ensure that dosages are within the safe range for all forms of medication. Question dosages that are too high or too low.
- NCLEX Tip: Some questions will ask you to calculate a particular dose of medication but ask the nurse for the appropriate action. These questions usually involve doses that are either too high or too low.
- Ensure that all measurements follow the same system. Convert from one system to another if needed.
- Parenteral administration of medications follow the protocol below:
- For pediatric patients, 1mL Tuberculin syringe is typically used. The values are rounded off to the nearest hundredths.
- For adult patients, 3mL standard syringes are used. Values are typically rounded off to the nearest tenths.
- Do not confuse the insulin syringe for the Tuberculin syringe.
Common Formulae for Dosage and Calculations
A. Dosage
Using the formula: D/S x Q, where:
D= desired dose
S= stock on hand or available strength of the solution
Q= quantity or volume of the medication available
Example:
1. The physician ordered a patient to receive 500 mg of mefenamic acid for pain. The nurse notes that the stocks currently available at the pharmacy comes only in 250mg tablets. How many tablets does the patient receive?
Formula: D/S x Q, where:
D= 500 mg
S= 250 mg
Q= I tablet
500 mg x 1 tablet = 2 tablet
250 mg
2. A pediatric patient was ordered to receive paracetamol syrup to lower his body temperature. The order reads 1250 mg every 6 hours. The medicine comes in preparation of 500 mg per 5 mL. How many mL of syrup is to be given to the child every 6 hours?
Formula: D/S x Q, where:
D= 1250 mg
S= 500 mg
Q= 5 mL
1250 mg x 5 mL = 12.5 mL
500 mg
B. Formula for IV Fluid Flow Rate
Using the formula:
Total volume x Drop Factor = Drops per minute or gtts
Time in Minutes
Example:
1. Mrs. Jefferson is to receive 125 mL of D5LR per hour over the next 8 hours. She is to use an IV tubing set with a drop factor of 10. How many drops per minute does the nurse need to infuse the IV fluid?
Formula:
Total volume x Drop Factor = Drops per minute or gtts
Time in Minutes
where:
Total Volume= 125 mL
Drop Factor= 10 gtts
Time= 60 minutes
125mL x 10 gtts= 21 gtts/minute
60 minutes
2. Jones ordered an elderly patient to be hooked on an infusion of 1000 cc of D5W. The first bottle is expected to run for 8 hours. If the IV tubing set that is prescribed for the patient has a drop factor of 15 gtts, how many drops per minute is the patient to receive over the next 8 hours?
Formula:
Total volume x Drop Factor = Drops per minute or gtts
Time in Minutes
where:
Total Volume= 1000 mL/cc
Drop Factor= 15 gtts
Time= 480 minutes
1000 cc x 15 gtts= 31 gtts/minute
480 minutes
C. Infusion Time for IV Fluids
Using the formula:
Total volume to be infused = Infusion time mL per hour to be infused
Example:
1. A patient who has severe thickness burns of the upper body is prescribed to be on a fluid replacement for the first few hours upon admission. The total computed amount of fluids to be administered to the patient is 4 liters, with an average of 500 ml needed to be infused per hour. How long would it take for the nurse to infuse all 4 liters of fluid?
Total volume to be infused= Infusion time mL per hour to be infused
Number of Hours
where:
Total Volume= 4 liters or 4000 mL
mL per hour= 500 mL
4000 mL = 8 hours
500 mL/hr
D. Total Number of mL per hour
Using the formula:
Total volume in mL= Number of mL to be infused per hour
Number of hours
Example:
1. A patient who has severe thickness burns of the upper body is prescribed to be on a fluid replacement. The total computed amount of fluids to be administered to the patient is 4 liters over a 6 and a half-hour time period. How many mL of fluid is the patient going to receive per hour?
Formula:
Total volume in mL= Number of mL to be infused per hour
Number of hours
where:
Total Volume= 4 liters or 4000 mL
Number of hours= 6.5 hours
4000 mL = 615.38mL per hour
6.5 hours
E. Calculating Drip Rate for Emergency Medications and Other Side Drips
Using a 2-step process, side drips can be computed to be administered:
A. How much medication per mL is to be administered.
The client is to receive a continuous infusion of heparin sodium via an infusion pump. The heparin should be administered at 1000 units per hour. The available stock comes in an IV bag of 500 mL of D5W mixed with 20,000 units. How many mL per hour is the nurse going to administer to give the patient the correct dose?
Solution:
1. Determine how many units of heparin comes per mL of fluid using the following formula:
Amount of medication in available solution= Medication per mL
Total Volume of Solution
20,000 units = 40 units/mL
500 mL
2. Calculate how many mL per hour the medication is supposed to flow or run:
Dose per hour desired = Infusion rate expressed
Concentration per mL
1000 units= 25 mL per hour
40 units
Answer: 25 mL per hour
B. How many mL per hour is to be administered per hour
Ms. Louis is a known diabetic being treated for the diabetic foot. Since his blood glucose levels need to be maintained at a certain level, he is to be hooked on an infusion pump to receive 10 units of insulin per hour. The stock comes in an IV bag of 100 mL of normal saline solution with 50 units of regular insulin. How many mL does the nurse need to administer per hour to give the patient the correct dose?
Solution:
1. Determine how many units of insulin comes per mL of fluid using the following formula:
Amount of medication in available solution= Medication per mL
Total Volume of Solution
50 units= 0.5 units/mL
100
2. Calculate how many mL per hour the medication is supposed to flow or run:
Dose per hour desired= Infusion rate expressed
Concentration per mL
10 units = 20 mL per hour
0.5 units/mL
Answer: 20 mL per hour
Reminders on Answering Questions on Dosage and Calculations
- For IV Infusion of Medications and Fluids:
-
-
- Monitor the flow rate of IV fluids and all other medications administered to the patient via the intravenous route.
- Calculations, especially when using an infusion pump to administer medications, should be carefully checked to ensure that errors are not made.
- When an infusion pump is used, bear in mind that these are calibrated regularly and the priority is monitoring the patient’s response to therapy.
- Normally, heparin and insulin are run continuously if the patient is hooked to an infusion pump. These medications run on a separate line with their own drip-rate calculated apart from the mainline.
- IV fluids are usually expressed to be administered in drops per minute (gtts/min). In pediatric patients, this is shown as microdrops per minute (mgtts/min).
- The number of drops per minute in an IV tubing set usually denotes 1 mL.
- Common drops per minute flow rate used in most nursing exams:
-
-
-
-
- Adult: 10 and 15 gtts/minute
- Pediatric: 60 mgtts/minute
-
-
-
- When answering questions involving the use of medicine cups, note that each cup has a maximum capacity of 30mL or fluids (1 ounce; 2 tablespoons).
- Medicine cups have calibrations that the nurse can use to measure the amount of fluid to be administered.
- When administering volumes below 5mL, especially for pediatric patients, the best method to measure it is through the use of a syringe.
See Also
Conclusion
Medication errors are one of the most common sources of complaints of patients about the care that they receive. The nurse is expected to not only administer medications on time but also know that the dosage given to the patient is correct and within the safe ranges. Calculations should be done accurately and carefully prior to administering drugs so that patient safety is maintained and the nurse provides the highest quality of care possible.
References:
- Arnoldussen, B., 2019. NCLEX-RN Drug Guide. 7th ed. United States of America: Kaplan Publishing.
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Colgrove, K. and Doherty, C., 2018. Pharmacology Success. 3rd ed. Philadelphia, PA, USA: F A Davis Co.
- Hinkle, J.L. & Cheever, K.H. (2018). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (14th ed.). Philadelphia: Wolters Kluwer.
- Potter, P.A., Perry, A.G., Stockert, P.A., & Hall, A.M. (2019). Essentials for Nursing Practice (9th ed.). St. Louis: Elsevier.