1.) 167 mL/hr.
Rationale: The nurse should divide the volume (1,000 mL) by the number of hours (6). This equals 166.6666. The nurse should round up if the number is greater than 5; therefore, the nurse should set the pump at 167 mL/hr.
Test-Taking Strategy: Focus on the subject, obtaining the mL per hour to be infused. Once the calculation is performed, the answer may be verified using a calculator. Ensure that the figure obtained is rounded off to the nearest whole number and it is realistic in a clinical setting.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
2.) 100 mL.
Rationale: The pump administers medication at a rate per hour; therefore, 100 mL would infuse over 1 hour.
Test-Taking Strategy: Focus on the subject, obtaining the mL per hour to be infused. Once the calculation is performed, the answer may be verified using a calculator. Ensure that the figure obtained is rounded off to the nearest whole number and it is realistic in a clinical setting.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
3.) 21
Use the intravenous (IV) flow rate formula.
Formula:
Total volume x Drop Factor = Drops per minute
Time in Minutes
1000mL x 15 gtts= 15,000 = 20.8 or 21gtts/min
720 mins 720 mins
Test-Taking Strategy: Focus on the subject, IV flowrates. Use the formula for calculating IV flow rates when answering the question. Once the calculation is performed, the answer may be verified using a calculator. Ensure that the figure obtained is rounded off to the nearest whole number and it is realistic in a clinical setting.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
4.) 8
Rationale: You must determine that 1 L equals 1000 mL. Next, use the formula for determining infusion time in hours.
Formula:
Total volume to be infused= Infusion time infused
mL per hour being infused
1000 mL = 8 hours
125 mL
Test-Taking Strategy: Focus on the subject, an intravenous infusion calculation. Read the question carefully, noting that the question is asking about infusion time in hours. First, convert 1 L to milliliters. Next, use the formula for determining infusion time in hours. Verify the answer using a calculator and make sure that the answer makes sense.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019).
5.) 16
Rationale: Calculation of this problem can be done using a 2- step process. First, you need to determine the amount of heparin sodium in 1 mL. The next step is to determine the infusion rate, or milliliters per hour.
Step 1:
Known amount of medication in solution= Amount of medication per mL
Total volume of diluent
20,000 units = 80 units/mL
250mL
Step 2:
Dose per hour desired=Infusion Rate in mL per hour
Concentration per mL
1300 units = 16.25 or 16 mL per hour
80 units/mL
Test-Taking Strategy: Focus on the subject, an IV flow rate. Read the question carefully, noting that 2 steps can be used to solve this medication problem. Follow the formula, verify the answer using a calculator, and make sure that the answer makes sense. Remember to round the answer to the nearest whole number.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019).
6.) 0.8mg
Rationale: Use the formula to calculate the correct dose.
Formula:
Desired dose in mL = mL per hour
Available stock
8 milligrams= 0.8 mL
10mg/mL
Test-Taking Strategy: Focus on the subject, a dosage calculation. Follow the formula for the calculation of the correct dose. Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
7.) 8
Rationale: Calculation of this problem can be done using a 2-step process. First, you need to determine the amount of regular insulin in 1 mL. The next step is to determine the infusion rate, or milliliters per hour.
Formula:
Step 1:
Known amount of medication in solution= Amount of medication per mL
Total volume of diluent
100 units= 1 unit/mL
100mL
Step 2:
Dose per hour desired= Infusion rate in mL per hour Concentration per mL
8 units= 8 mL/hr
1 units/mL
Test-Taking Strategy: Focus on the subject, an IV flow rate. Read the question carefully, noting that 2 steps can be used to solve this medication problem. . Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense. These steps can be used for similar medication problems related to the administration of heparin sodium or regular insulin by IV infusion.
Review: Medication calculations
Level of Cognitive Ability: Analyzing
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019).
8.) 280-560 mg per day
Rationale: Use the following formula to calculate for the safe dosage:
Weighs = 11.2 kg
120 mg = 8 hours
SDR = 25-50 mg/kg/day
Mg/day = 25mg/1 kg/day X 11.2 kg/1 = 280 mg/day
Mg/day = 50mg/1 kg/day X 11.2kg/1 = 560 mg/day
SDR = 280-560 mg/day
Test-Taking Strategy: Focus on the subject, a safe dose rate for a pediatric patient. Read the question carefully, noting that the question asks for a range involving minimum and maximum dosage. Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations for pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
9.) 93.3 mg to 186.7 mg per dose
Rationale: Use the following formula to calculate for the safe dosage:
Weighs = 11.2 kg
120 mg = 8 hours
SDR = 280-560 mg/day
1 day = 24 hours
Mg/dose = 280mg/day X day/24 hr X 8 hrs/dose = 93.3 mg/dose
Mg/dose = 560 mg/day X day/24 hrs X 8 hrs/dose = 186.7 mg/dose
Test-Taking Strategy: Focus on the subject, a safe dose rate for a pediatric patient. Read the question carefully, noting that the question asks for a range involving minimum and maximum dosage. . Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations for pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
10.) C
Rationale: Calculate the intended dosage for the child using the following formula:
Step 1: Convert pounds to kilograms
48 pounds = 1 kilogram = 48 = 21.81 kg
1 pound 2.2 pounds 2.2 kg
Step 2: Calculate the dosage for 1 day
5 mg/kg/day x 21.81 kg = 109.05 mg per day
Step 3: Divide the daily dose into 2 equal doses
109.05 mg/2 = 54.53 or 55 mg
Test-Taking Strategy: Focus on the subject, a safe dose rate for a pediatric patient in a given time period. Read the question carefully, noting that the question asks for a range involving minimum and maximum dosage. Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations for pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
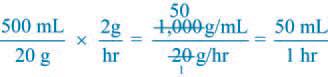
11.) 50 mL
Rationale: Refer to the solution below:
Test-Taking Strategy: Recall basic calculation of desired doses of magnesium sulfate for a pregnant patient. Calculate the desired dose, and check the answers with a calculator to confirm accuracy.
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Arnoldussen (2019).
12.) 8:00 am
Rationale: If 10 mg were administered at 10:00 a.m. and 12:00 p.m. and then 20 mg were administered at 4:00 p.m., 8:00 p.m., 10:00 p.m., 12:00 a.m., 4:00 a.m., and 8:00 a.m., the dose at 8:00 a.m. reached the maximum oral dose of 120 mg/day.
Test-Taking Strategy: Count the number of times a dose was provided to the client throughout the day, considering the maximum safe dosage allowed.
Level of Cognitive Ability: Analyzing
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Arnoldussen (2019).
13.) 135 mg.
Rationale: The recommended dose of ampicillin for a neonate is 100 mg/kg/dose. First, determine the neonate’s weight in kilograms, and then multiply the kilograms by 100 mg. The nurse should use this formula:
1,000 g = 1 kg
1,350 g = 1.35 kg
100 mg x 1.35 kg = 135 mg/kg
Test-Taking Strategy: Focus on the subject, a safe dose rate for a pediatric patient using the milligram per kilogram of body weight. Read the question carefully, noting that the question asks for a range involving minimum and maximum dosage. Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations for pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
14.) 240 calories
Rationale: The total number of calories is computed using the following steps:
Step 1: Convert 45 ml to ounces
30 ml= 1 ounce
45 ml= 1.5 ounces
Step 2: Calculate the total number of ounces consumed in 8 feedings
1.5 ounces x 8 feedings= 12 ounces
Step 3: Calculate the total calories in 1 day.
1 ounce= 20 calories
12 ounces = 240 calories
Test-Taking Strategy: Focus on basic medical mathematics to calculate for total caloric intake.
Review: Caloric intake of pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
15.) 0.03 mg
Rationale: The dosage is calculated as follows:
Step 1: Convert pounds to kilograms
5.5 lbs / 2.2= 2.95 kg
Step 2: Calculate the dose based on mg/k
0.01mg per kg x 2.95 kg
= 0.029mg or 0.03mg
Test-Taking Strategy: Focus on the subject, a safe dose rate for a pediatric patient using the milligram per kilogram of body weight. Read the question carefully, noting that the question asks for a range involving minimum and maximum dosage. Once the calculation is performed, verify the answer using a calculator and make sure that the answer makes sense.
Review: Medication calculations for pediatric patients
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
16.) d
Rationale: Convert 1 g to milligrams. In the metric system, to convert larger to smaller, multiply by 1000 or move the decimal point 3 places to the right: 1 g = 1000mg
Formula:
Desired dosage x Volume
Available stock
125 mg x 7.4mL = 0.925mL
1000 mg
Test-Taking Strategy: Focus on the subject, milliliters per dose. Convert grams to milligrams first. Next, use the formula to determine the correct dose, knowing that when reconstituted, 1000 mg= 7.4 mL. Verify the answer using a calculator.
Review: Medication calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
17.) c
Rationale: Rationale: Calculate the daily dosage by weight first:
8mcg=day x 7.2 kg = 57.6mcg per day
The HCP prescribes digoxin twice daily; 2 doses in 24 hours will be administered: 57.6 mcg per day/2 doses = 28.8 mcg for each dose
Test-Taking Strategy: Focus on the subject, mg per dose, and note that the question states twice daily and each dose. Calculate the dosage per day by weight first, and then determine the micrograms per each dose by dividing the total daily dose by 2. Verify the answer using a calculator.
Review: Medication calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Hockenberry, Wilson (2015), p. 914.
18.) d
Rationale: Use the medication calculation formula.
Formula:
Desired dosage x Volume
Available stock
1,000,000 units x 2mL = 1.7mL per dose
1,200,000
Test-Taking Strategy: Focus on the subject, milliliters per dose. Use the formula to determine the correct dose, and verify the answer using a calculator.
Review: Medication calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
19.) 1.5mL
Rationale: Use the formula for calculating the medication dose.
Formula:
Desired dosage x Volume
Available stock
0.6 milligrams x 1mL = 1.5mL per dose
0.4 milligrams
Test-Taking Strategy: Focus on the subject, the milliliters to be administered. Note that the medication label indicates that there is 0.4 mg/mL. Use the formula to determine the correct dose, and verify the answer using a calculator.
Review: Medication administration guidelines
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
20.) 6.8mL per dose
Rationale: The first step is to determine the body weight in kilograms. 60 pounds
divided by the 2.2 conversion factor is 27.272, or 27.27 kg. Multiply 27.27 times 10 to find the milligrams, which results in 272.2 or 272 mg of medication each 24 hours. Divide 272 mg by 2 to determine the amount of medication to be administered each dosing time; this equals 136 mg per dose.
Test-Taking Strategy: Focus on the subject, the milliliters to be administered. Note that the medication label indicates that there is 0.4 mg/mL. Use the formula to determine the correct dose, and verify the answer using a calculator.
Review: Medication administration guidelines
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
21.) 62 mL per hour.
Rationale: The nurse should decrease the rate by 5 mL every hour. In 3 hours it should be decreased by 15 mL. The nurse should subtract 15 mL from 77 mL to get 62 mL.
Test-Taking Strategy: Focus on basic medical mathematics to calculate for mL per hour rate after the prescribed reduction in flow rate.
Review: Medication administration guidelines; IV fluid flow rates
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
22.) 8.2mL per hour
Rationale: Calculate using the following steps.
Step 1: Convert pounds to kilograms
9 pounds x 1 kilogram = 4.1kg
2.2 pounds
Step 2: Calculate mL per hour based on weight.
2mL/kg x 4.1kg = 8.2mL per hour
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage based on mL per kg of body weight computation.
Review: Safe medication computation
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
23.) 11.3 mg
Rationale: Calculate using the following steps.
Step 1: Convert pounds to kilogram
25 pounds x 1 kilogram = 11.3kg
2.2 pounds
Step 2: Calculate mg per day based on weight.
2mg/day x 11.3kg = 22.7mg per day
Step 3: Divide in 2 equal doses.
22.7mg / 2 doses = 11.3mg per dose
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosafe based on mg per kg of body weight computation.
Review: Safe medication computation
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
24.) 200 mcg
Rationale: Using the following steps, compute for the dosage required:
Step 1: Calculate the number of milligrams per mL.
50mg = 1mg = 0.2 mg
250mL = 5mL = 1mL
Step 2: Calculate the number of micrograms in each milligram:
0.2 mg x 1,000 mcg =200 mcg
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
25.) 0.85 mL
Rationale: Calculate for the dosage using the following steps:
Step 1: First convert pounds (lb) to kilograms (kg) by using the formula:
1 kg = 2.2 lb [187 lb ÷ 2.2 = 85 kg].
The physician’s order is for the client to receive enoxaparin (Lovenox) 1 mg/kg. Therefore, the client is to receive 85 mg. The desired dose in milliliters then can be calculated by using the formula of desired dose (D) divided by dose or strength of dose on hand (H) times volume (V).
Step 2: Calculate the dose:
85 (mg) Å~ 0.3 mL = 25.5 mg/mL
25.5 mg ÷ 30 = 0.85 mL.
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
26.) 1,000 mg
Rationale: The client weighs 220 pounds. Convert weight to kilograms by dividing by 2.2 (220 ÷ 2.2 = 100 kg). To find the amount for each dose, multiply 100 kg times 10 mg, which equals 1,000 mg per dose.
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
27.) 7.5mL
Rationale: The dose is calculated as follows:
300 mg/X = 200 mg/5 mL
X = 7.5 mL
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
28.) 0.7 mL
Rationale: The dose is calculated as follows:
10 mg : X mL = 15 mg : 1 mL
15 mg × X mL = 10 mg × 1 mL
15X = 10
X = 0.6667
X = 0.67 mL.
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
29.) 25 ggt/min.
Rationale: To administer I.V. fluids at 100 mL/hour using tubing that has a drip factor of 15gtt/mL, the nurse should use the following formula:
100 mL/60 minutes × 15 gtts/1 mL = 25 gtt/minute.
Test-Taking Strategy: Focus on the subject, IV flowrates. Use the formula for calculating IV flow rates when answering the question. Once the calculation is performed, the answer may be verified using a calculator. Ensure that the figure obtained is rounded off to the nearest whole number and it is realistic in a clinical setting.
Review: Intravenous infusion calculations
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter & Stockert (2019).
30.) 4 tablets
Rationale: To administer 2 g sulfasalazine (Azulfi dine), the nurse will need to administer 4 tablets. The following formula is used to calculate the correct dosage:
Step 1: Convert grams into milligrams:
1 g/1,000 mg = 2 g/X mg
X = 2,000 mg.
Step 2: Calculate how many tablets is needed for the computed dose
2,000 mg/X tablets = 500 mg/1 tablet
X = 4 tablets.
Test-Taking Strategy: Focus on basic medical mathematics to calculate for the dosage.
Review: Medication administration guidelines
Level of Cognitive Ability: Analyzing; Applying
Client Need: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
References: Perry, Potter & Stockert (2019); Colgrove & Doherty (2018); Arnoldussen (2019).
BONUS SECTION: Therapeutic Levels of Common Drugs
| Generic Name | Trade Name | Use | Therapeutic Level |
| Carbamazepine | Tegretol | Anti-convulsant | 4-10 mcg/mL |
| Digoxin | Lanoxin | Cardiac Glycoside | 0.8-2.0 ng.mL |
| Gentamycin | Garamycin | Broad Spectrum Antibiotic | 5-10 mcg/mL (during peak); <2.0mcg/mL (valley) |
| Lithium | Eskalith | Antimanic | 0.8-1.5 mEq/L; critical 2.0 mEq/L |
| Phenobarbital | Solfoton | Anti-anxiety; anti-seizure | 15-40 mcg/mL |
| Phenytoin | Dilantin | Anti-convulsant | 10-20 mcg/dL |
| Theophylline | Aminophylline | Bronchodilator | 10-20 mcg/dL |
| Tobramycin | Tobrex | Aminoglycoside; used to treat Gram negative infections | 5-10 mcg/mL (peak); 0.5-2.0 mcg/mL (valley) |
| Valproic Acid | Depakene; Depakote | Anti-seizure | 50-100 mcg/mL |
| Vancomycin | Vancocin | Broad spectrum antibiotic; used primarily to treat Methicillin-resistant staphylococcus aureus | 20-40 mcg/mL (peak); 5-15 mcg/mL (trough) |
References
- Arnoldussen, B., 2019. NCLEX-RN Drug Guide. 7th ed. United States of America: Kaplan Publishing.
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Colgrove, K. and Doherty, C., 2018. Pharmacology Success. 3rd ed. Philadelphia, PA, USA: F A Davis Co.
- Hinkle, J.L. & Cheever, K.H. (2018). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (14th ed.). Philadelphia: Wolters Kluwer.
- Potter, P.A., Perry, A.G., Stockert, P.A., & Hall, A.M. (2019). Essentials for Nursing Practice (9th ed.). St. Louis: Elsevier.








Number 23 is wrong, if you are rounding to one decimal place.
Very helpful article love it.
Yes, love this concern good article
i concur with you