Nursing care of the newborn patient requires additional skills and knowledge for the nurse to efficiently address the needs of these patients. Textbooks define the newborn stage as lasting from anywhere between the moment of birth until the first four weeks of life, or 28 days after delivery.
While most deliveries are considered a routine procedure (either via NSD or Caesarian section), some newborns may present with risk factors and other symptoms that require immediate intervention. Because of this, the nurse who is responsible for the care of newborns should be knowledgeable about how to manage these patients as they transition from intrauterine to extrauterine life.
The American Academy of Pediatrics and the American Congress of Obstetricians and Gynecologists have included in their guidelines several levels of care that involve the neonate. These levels are:
- Level 1- or basic neonatal care, involves the meeting of minimum requirements by any facility that performs birthing services. These include having the essential trained personnel and equipment to perform neonatal resuscitation and stabilization. They should also have the capacity to coordinate referrals for newborns needing more specialized care.
- Level II- are birthing facilities that are reserved for newborns who have been stabilized and are moderately ill, born on or a few weeks over 32 weeks of gestation. They may weigh a little more than 1500 grams at birth and may need to be immediately transported to specialized facilities urgently. While most of these newborns may be delivered under uncomplicated conditions, their weights and ages of gestation may indicate a need for more specialized care.
- Level III- are facilities that cater to caring for infants born at less than 32 weeks of gestation, and are usually categorized as pre-term. These facilities should have practitioners who have training and experience in providing neonatal life support, physiologic monitoring, imaging, and nutrition. Nurses who are assigned at these facilities should also have the skills to provide psychosocial care to the family of the infants.
- Level IV- are facilities that are capable of providing highly specialized care to patients with critical conditions as well as those who need immediate aggressive therapy for complex conditions such as congenital cardiac malformations, spinal cord anomalies, and other life-threatening conditions.
Nurses who are caring for neonates, regardless of the level of care required, should have the necessary training to care for infants. These requirements include neonatal resuscitation certification and training, which must be renewed every two years. Furthermore, other skills related to postpartum care and newborn resuscitation should be updated, such as:
- Temperature monitoring and control
- Pulse oximetry monitoring
- Provision of care for the infant under warmers/warming equipment
- Caring for infants with orogastric tubes and IV lines
- Monitoring infants under isolettes or incubators
There are several indicators of a newborn’s wellbeing that the nurse needs to take into consideration when assessing these patients and planning for care. First among these is the APGAR Score.
What is the APGAR Score?
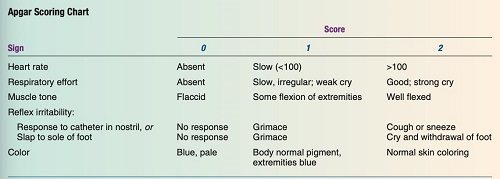
The APGAR Score is an acronym that denotes specific areas of assessment that must be evaluated between the first and fifth minutes of life. Individual parameters are scored. The highest possible score for each of the five areas is 2, while the lowest possible score is 0. The following is how scoring is interpreted:
- 0-3 points: the score indicates that the child may be in danger; immediate resuscitation is needed; the child may need to be transferred to an urgent care facility
- 4–6 points: the assessment may indicate potential airway or breathing issues, and there is a need for oxygen supplementation
- 7-10 points: a favorable finding and usually indicates that the infant is in good health.
The APGAR Score follows the table below in the assessment of the newborn. Note that assessments are done immediately after birth (first minute of life) and 5 minutes after to serve as baseline data and indicate the infant’s adjustment to extrauterine life. Findings are documented, and any indicators that need immediate attention are reported to the physician for immediate attention.
Assessing for General Infant Wellbeing
The most critical period immediately following the infant’s birth is between the first few minutes and at least the first 8 hours of life. This is due to the neonate gradually transitioning and adjusting from life inside the uterus to life outside the uterus. The lungs, which the placenta had previously oxygenated, are now being oxygenated as the infant breathes.
Apart from this significant adjustment, the infant is also suddenly exposed to colder temperatures outside the warm environment of the uterus, and his connection to his mother’s nutrient flow via the umbilical cord is cut. Therefore, the nurse needs to conduct a thorough assessment to determine priority nursing care, rule out potential problems, and ensure that the neonate’s transition to extrauterine life will go as smoothly as possible.
A. Respiratory Assessment
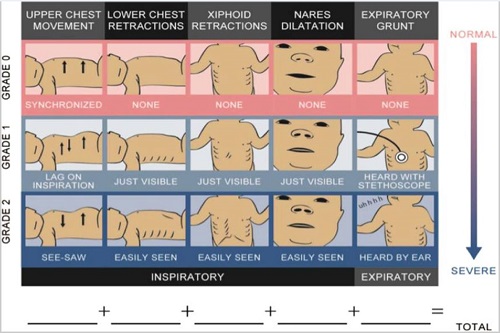
Considered to be one of the top priorities in caring for the newborn, assessing the infant’s respiratory status goes beyond the APGAR scoring. Immediate evaluation of respiration is performed using the Silverman and Andersen Index, which evaluates the infant using five criteria:
- Chest movements- should be symmetrical during respiration; spontaneous; asymmetrical movements are scored 1 or 2 depending on the severity
- Intercostal retractions- should not be present (score of 0)
- Xiphoid retractions
- Dilation of the nares during respirations- indicative of the difficulty in breathing (infants are obligatory nose breathers)
- Expiratory grunting- may indicate airway patency problems.
While the highest score for APGAR is between 7-10 and indicates good fetal well-being, the Silverman and Andersen Index scoring is the opposite. A score of 0 indicates that the fetus is not experiencing any respiratory distress, while a score between 7-10 indicates severe respiratory distress. (see figures below)
B. Physical Examination
A thorough physical examination is performed on the infant to identify any observable conditions or physical deformities that may necessitate immediate intervention or referral to a more specialized facility. When assessing the newborn physically, keep the following points in mind:
- Assessment should be done quickly to avoid overexposing the newborn
- Respiratory assessment should be the first to be done
- Determine the height (in cm) and weight of the infant as this helps determine maturity compared to average ranges for age of gestation.
- When weighing newborn, ensure that this is done at the same time each day to help note for any abnormal weight losses or gains
- Blood testing may be required to be performed such as the heel-stick test to determine blood glucose, hemoglobin, hematocrit, bilirubin and other parameters
- Behavioral capacity assessment for the newborn may also be done to help determine ability of the infant to interact with the people around them.
C. Immediate Care of the Newborn Upon Birth
Ideally, the newborn receives immediate care in a separate area from his mother in the birthing suite/facility. This area is typically equipped with a heated table, warming blankets or other related equipment, a resuscitation set, eye ointment, suction equipment, and other relevant materials. In order to provide immediate care for the newborn, the following actions are taken:
- Placing an identification band around the newborn’s arm or leg and creating his own registry. This aids in the identification of the newborn and the prevention of infant switching.
- Footprints of the newborn are taken and kept for identification. In some cases, additional copies may be given to parents/families who request to have it.
- Recording of the name of the infant in his EMR. If the infant does not have a name yet, he/she may be referred as Baby Boy/Girl (last name of mother/parents).
- Recording of APGAR Score, Silverman and Anderson Sore, birth weight, length and other anthropometric measurements, vital signs.
- Provision of immediate care such as immunizations, bathing, swaddling, placement under bili-light/warmer and postural drainage.
- Feedings may be given to the infant depending on preference of the parents. Breastfed infants to feed immediately when the mother is able. Bottle fed infants are normally fed after 2-4 hours upon delivery.
- Rooming-in of the infant with the mother is highly encouraged after 6-8 hours to promote bonding.
Other Expected Newborn Assessment Findings
Apart from assessing vital signs, caring for the newborn immediately after birth, the nurse also needs to take note of the following assessment findings that may be present among the newborn patients. While some of these findings are expected and may return to normal a few days after birth, some may need to be reported to the physician for further evaluation and management.
A. Head
- The infant’s head is roughly one-fourth the length of the entire body, and the sutures are still palpable. Sutures are expected to be completed in 6 and 18 months, respectively.
- Due to passage through the birth canal, head molding may still be present. It should not, however, be widened. Molding is expected to subside 72 hours after birth.
- Birth trauma masses may also be present and are expected to go away in a few days:
- Caput succedaneum is an edema of the soft tissues that extends over the bone and crosses suture lines.
- Cephalhematoma- a type of swelling that is caused by bleeding into an area between the one and the periosteum. However, this bleeding does not cross over suture lines and is reabsorbed into the body over a 6-week period.
- Head lag is a common finding when pulling the newborn to a sitting position at least 3 months of age. The infant is expected to be able to lift the head slightly and turn the head side to side when placed on a prone position
-
- The spine of the infant should appear to be straight, while the posture is slightly flexed.
- Movements should be well-coordinated and sporadic. Hypotonic or hypertonic movements may indicate possible central nervous system damage.
- No hair tufts or depression should be seen along the spinal column. Presence of these findings may indicate spina bifida or a possible opening of the spinal column.
- Extremities should have a symmetrical and full range of motion.
- Fists of the infant usually are clenched, with all 10 fingers separating and fanning out when the palms are open.
- Legs appear to be bowed initially and corrects over the first few years of life.
- Gluteal folds are even.
- Creases are present along the soles of the feet and pulses are palpable in the brachial, radial and femoral sites.B. Eyes
- The eyes should be clear and symmetrical.
- (+) PERRLA
- Blink reflex should be assessed and present.
- The infant may appear to be initially cross-eyed due to weak extraocular muscles. This will resolve over time.
- Red eye reflex is also present, and the infant is also able to track and fix his eyes on an object momentarily.
- Immediately after birth, the eyelids may appear to be slightly edematous due to the pressure on the infant’s face during the birthing process. This may also be due to the effects of the eye ointment applied in the immediate care after delivery.
C. Ears
- The ears should be symmetrical, cartilage is firm and recoils
- The top of the pinna should be on or above the imaginary line drawn from the outer canthus of the eyes.
- Note that low-set ears may be indicative of a renal problem, Down syndrome or other genetic abnormalities.
D. Nose
- The nose may be flat or broad and infants are obligatory nose breathers.
- Some infants may occasionally sneeze to remove any obstructions in the nasal passages.
- Nares should not flare and must be patent at all times. Flaring nares may indicate respiratory distress.
E. Mouth
- Oral mucosa should appear pink and moist, with both hard and soft palates intact.
- Presence of Epstein’s pearls may be seen on hard palate. These are tiny white cysts and disappear over time.
- The uvula should be positioned in the midline of the mouth, the tongue moving freely and has a short frenulum.
- Rooting and gag reflex should be present and the infant should present with a good sucking and swallowing reflex.
F. Neck
- The neck should be able to hold the head in the midline position and is short and thick in appearance.
- There should be a good range of motion, and the infant displays an ability to flex and extend the neck simultaneously.
- Torticollis may be seen in some infants. This is the inclination of the head to one side of the body as a result of the muscular contractions along that side of the neck. It is expected to subside over time.
G. Chest
- Chest anteroposterior and lateral diameters should be about equal at birth, giving the infant’s chest a circular appearance.
- The chest measures approximately 30-33cm at birth.
- Respirations should be diaphragmatic, where the chest and abdomen should rise and fall synchronously. A seesaw pattern of respirations may indicate distress and needs immediate interventions.
- Bronchial sounds should be heard upon auscultation.
- Nipples should be prominent and appear to be slightly edematous. Some infants may have milky secretions on their nipples when expressed. This is termed as witch’s milk and is a normal occurrence due to the influence of maternal hormones in utero.
H. Skin
- The infant’s skin should appear to be pinkish-red among light-skinned newborns and pinkish-brown or pinkish-yellow among dark-skinned infants.
- Vernix caseosa, a cheesy-white substance covering the infant’s body that protects the skin inside the uterus, may be seen more prominent along the skin folds. This may be more pronounced among preterm infants and less evident for infants above 42 weeks of gestation.
- Lanugo, fine downy hair, may be seen more prominent on the infant’s back, along the arms and the legs. This is normal and the infant sheds this over time.
- White sebaceous glands called milia may also be seen to appear on areas of the face such as the nose, forehead and chin. These glands may reduce in size and disappear in the first few weeks of life.
- Post mature newborns may appear to have dry skin and peeling is commonly seen among them.
- Premature newborns may present with plethoric coloring. This is characterized by dark red coloration of some areas of the skin and maybe secondary to over oxygenation upon delivery. This coloring will resolve after a few weeks.
- Cyanosis may be noted in the first few hours after birth, specifically acrocyanosis or peripheral cyanosis of the hands and feet. This usually resolves during the first two weeks of life.
- Good skin turgor should be noted, as this indicates hydration status of the infant. Assessment of skin turgor may be done over the abdomen.
- Some infants may also be seen with various birthmarks, which may be a normal assessment finding.
- Harlequin Sign, a deep pink or red coloration seen on one side of the body while the other side may remain normal in color or turn pale, may be observed. This is due to the shunting of the blood from one side of the body to the dependent portion and may indicate a cardiac problem or a septic condition. Presence of this sign needs to be reported immediately.
I. Abdomen
- The umbilical cord of the infant should have 3 vessels: 1 vein and 2 arteries. Any finding that is not within this range should be reported to the physician immediately as it may indicate intrauterine fetal growth restriction (IUGR), genetic abnormalities or congenital heart an0malies.
- The cord should be assessed for bleeding and any odor to determine presence of infections. Infected cord should be treated with antibiotics as prescribed.
- Assess for presence of abdominal distension, noting for presence of masses, obstruction or hernia. Report these findings to the physician right away.
- Bowel sounds should be present within the first hour after birth.
- Infant should also be able to pass the meconium or the first stool within the first 24 hours of extrauterine life.
J. Genitals
- For female infants:
- Labia may initially appear to be swollen and the clitoris is enlarged.
- Thick, white mucus drainage may be seen and is a normal finding.
- Blood-tinged mucus, also called pseudomenstruation, may be seen among infants. This is due to the withdrawal of the maternal estrogen upon delivery. It is a normal finding.
- In some infants, a hymen tag may be visible.
- For male infants:
- The prepuce or the foreskin covers the glans penis.
- The scrotum may also appear to be edematous and testes may retract when the infant is exposed to colder temperatures.
- Some infants may have one or both testes partially descended within the first few weeks of life, while some may have one of the testes undescended.
J. Spine and Extremities
Nursing Priorities in Caring for Newborn Infants
The newborn infant and the mother are treated as individual patients after delivery and must receive individualized care. Priority of caring for the infant focuses on facilitating his adaptation to extrauterine life, maintaining body temperature within normal ranges, preventing any complications related to adjustment to the outside environment, and ensuring that the family can care for the infant effectively.
In this regard, the nurse must include the family in planning care for the child after discharge and impart with them information that would help maintain fetal well-being. The following nursing diagnoses and care goals may be included in the immediate care of the newborn.
Newborn Nursing Diagnosis
- Risk for Impaired Gas Exchange
- Risk for Altered Body Temperature
- Ineffective Thermoregulation
1. Risk for Impaired Gas Exchange
Risk for impaired gas exchange related to: (the related factors may include but are not limited to: antepartal stress, excessive production of mucus in the airways, stress due to cold environment, improper suctioning of secretions; physical deformities in the airway).
Goal of care: The infant is expected to be free from signs of respiratory distress.
Nursing Interventions:
- Determine the APGAR Score on the first and fifth minutes of life and record to help determine if there is a need for oxygen resuscitation measures.
- Determine if there are any other prenatal conditions or complications which may contribute to infant respiratory distress and report to the physician immediately so that proper steps may be taken to ensure that the infant would not suffer from further complications.
- Clear the airway from secretions, ensuring to apply gentle suctioning to prevent damage to airway passages.
- Monitor the apical pulse of the infant during suctioning because suctioning may stimulate the vagal nerve and cause bradycardia. If the infant becomes bradycardic, stop the suction and report to the pediatrician.
- Ensure that the infant is dry and swaddled comfortably. If the infant is roomed in, encourage the family to hold him or place the infant under a warmer to help decrease the effects of cold stress on him.
- Promote postural drainage by placing the infant in a modified Trendelenburg position at an angle of 10 degrees to help drain mucus from the airway through gravity.
2. Risk for Altered Body Temperature
Risk for altered body temperature related to: (choose one or more from the following, or indicate risk factor identified upon assessment: inability of the infant to have chills, imbalance in body surface area compared to infant weight, decreased amounts of subcutaneous fats, thinner epidermal layer, immature thermoregulation).
Goal of care: The infant would be free from signs of cold stress; the infant would be able to manifest improve thermoregulation.
Nursing Interventions:
- Assess for the presence of fetal distress or hypoxia since this is normally seen upon infants who experience heat loss due to evaporation and conduction.
- Ensure that the head of the infant is dry and he is wrapped in a warm blanket.
- Ensure that the child does not come in contact with cold objects and drafts such as air from the AC unit, cold stethoscope and exposing a body part unnecessarily.
- Determine the range of temperature that can be considered ambient. Minimize the number of airflows and if necessary, limit the use of air-conditioning units since a colder environment may increase the oxygen consumption of the infant.
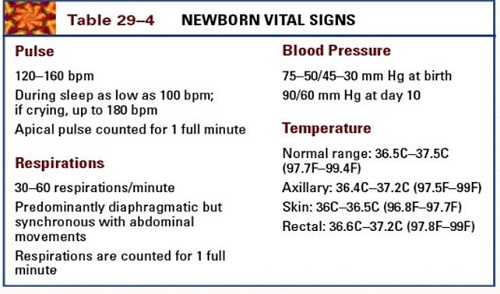
- Maintain body temperature within the normal range.
3. Ineffective Thermoregulation
Ineffective thermoregulation related to exposure to draft and cold environment secondary to being undressed/swaddled as evidenced by neonatal temperature below the normal range, increased respirations and heart rate.
Goal of care: The infant’s body temperature would be returned and maintained within the normal range.
Nursing Interventions:
- Maintain a neutral thermal environment to determine if the infant’s change in body temperature is caused by the immediate environment or due to other causes.
- Monitor the infant’s vital signs frequently to determine changes that may warrant immediate intervention.
- Avoid exposing infants to drafts, keeping them away from air-conditioning units and doorways. This intervention would help keep a stable temperature around the infant, reducing the risk for further problems in thermoregulation.
- Dress or swaddle the infant in warm clothing, ensuring that there are also coverings on the head and extremities to help keep warm and avoid cold.
- Place the infant under bili-light if needed, taking care to cover the eyes, genitals and other delicate areas of the body to add more warmth and to help maintain a temperature within normal range.
- Encourage the mother and other family members to hold the infant when needed to help maintain temperatures within the normal range since their body warmth can also contribute to warming the infant.
References
- Butkus, S. C. (2015). Maternal-neonatal nursing made incredibly easy! Third edition. Philadelphia, [Pa.]: Wolters Kluwer.
- De Sevo, M. (2016). Maternal and Newborn Success (3rd ed.). FA Davis Company.
- Flagg. (2017). Maternal and child health nursing (8th ed.). Lippincott Williams and Wilkins.
- Hedstrom, A. B., Gove, N. E., Mayock, D. E., & Batra, M. (2018). Performance of the Silverman Andersen Respiratory Severity Score in predicting PCO2 and respiratory support in newborns: a prospective cohort study. Journal of perinatology : official journal of the California Perinatal Association, 38(5), 505–511. https://doi.org/10.1038/s41372-018-0049-3
- Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., Wilson, D., Alden, K. R., & Cashion, M. C. (2017). Maternal child nursing care (6th ed.). Mosby.
- Pillitteri, A. (2014). Maternal & child health nursing: Care of the childbearing & childrearing family. Lippincott Williams and Wilkins. Wolters-Kluwer.








