Percutaneous Endoscopic Gastrostomy, or more commonly known as PEG, is a form of nutritional intervention implemented for patients who have conditions that render them unable to take nutrients orally.
Apart from PEG tubes, other forms of tube feedings are recommended for patients depending on the location and severity of their health problems. Regardless of the type and where these tubes are placed, the main goal of therapy is to ensure that patients’ nutritional needs are met.
Depending on their diagnoses, treatment plan, and general state of health, patients’ needs for various nutrients and vitamins can be met through oral or tube feedings.
Caloric needs are calculated based on the metabolic demands of the patient. Approximately 25kcal/kg of body weight is used to calculate how much would be given to the patient. These are usually divided into 4-6 feedings at an average volume of 300-500 cc; specific macronutrient volumes are computed as follows:
- Carbohydrates- 4 grams/kg per day, with a target of blood sugar levels below 180mg/dL. This amount may be lowered for patients with higher blood sugar levels.
- Proteins and amino acids- 1 to 1.8 grams/kg per day, depending on renal health, need for tissue repair, and overall nutritional status. Patients with renal or liver problems may be recommended to take lower levels than these.
- Fats and lipids- 0.7 to 1.5. grams/kg per day.
Patients who require PEG or other forms of enteral feedings should start the therapy as soon as it is determined. The decision to start tube feeding a patient may be due to any of the following conditions:
- Anatomic irregularities in the structure of the mouth, esophagus, or the stomach;
- Problems related to swallowing, which increases the risk for choking and aspiration;
- Inability to take food orally, which is secondary to other health conditions; and
- As preparation for surgical interventions involving the GI tract.
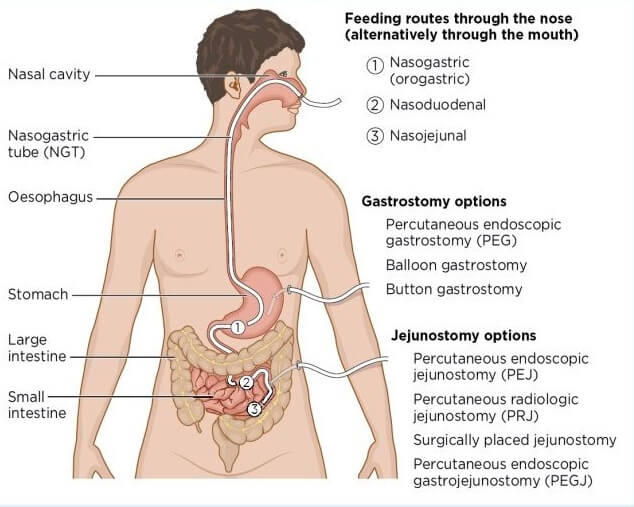
Several types of tube feedings can be prescribed for patients, such as nasogastric, nasojejunal, gastrostomy tubes (i.e., PEG tubes and RIG tubes), and jejunostomy tubes. The type of tubes used for a patient is determined based on several factors and the length of time they are used as access sites for feeding. The table below summarizes this:
| Type of Tube Feeding | Location | Purpose | Duration of Use |
| Nasogastric (NG) tube | Inserted through the nose, passing through the esophagus and into the stomach. | Enteral feedings; sometimes, the tube is used to decompress the stomach. | Short-term tube feeding needs not to exceed six to eight weeks. |
| Nasojejunal (NJ) tube | Inserted through the nose, passing by the esophagus and the stomach and straight into the small intestine. | Used as an alternative to NG tube when the patient cannot tolerate feeding through the stomach, normally done post gastric surgery. | In most cases, this is for short-term use (6-8 weeks) but may be extended when the patient needs more prolonged enteral feeding. |
Gastrostomy tubes
|
An opening is created directly into the stomach through a small incision in the abdomen. | Used for patients with complicated health conditions where other means of providing nutrients into the body is not feasible (i.e., gangrene or cancer of the stomach, obstruction) | Long term enteral feeding |
| Jejunostomy tube (PEG-J or JEJ) | Inserted through the stomach and into the small intestine (jejunum). Another way may be done by inserting the tube directly through a small incision in the abdomen where the jejunum is | Semi-permanent access for the patient who has had difficulty with gastroparesis, nausea, vomiting, or previous intolerance to gastric feeding.
|
Semi-permanent, 8 weeks up. |
Gastrostomy Tubes
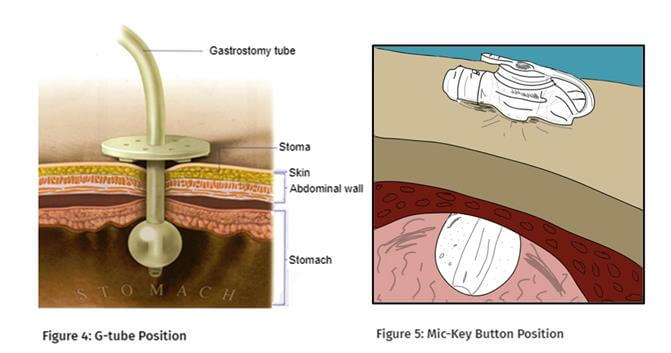
There are two sub-types for tubing inserted surgically to provide access for nutrition: gastrostomy and jejunostomy tubes. The most common among gastrostomy tubes is the PEG or percutaneous endoscopic gastrostomy.
The PEG Tube
This access is created surgically and under the guidance of an endoscope, providing long-term access to the patient’s gastric region. One of the most common reasons for physicians choosing the PEG over other surgically-created access types is that it can be used as early as four hours after it is created.
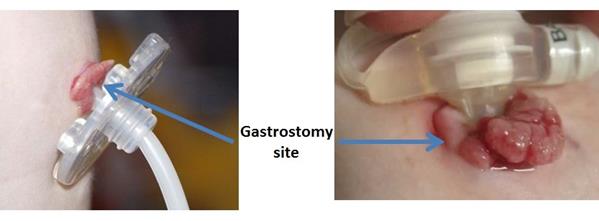
There are several parts of the PEG tube that you must be familiar with when caring for patients with this access. These include:
- The PEG tube itself;
- 2 small discs are placed on each side of the stoma (or opening into the abdominal wall). These discs are used to secure the stoma in place and also prevent the tube from falling.
- Tube clamp
- Button (a device used while the stoma is being healed) can also be placed on the site to help make feedings easier.
In some instances where there is the difficulty maintaining the tube and the discs in place, an adhesive device may be used to attach the tube’s side that touches the skin and on the abdominal wall. The tube is taped in place in between feedings. However, the adhesive may cause skin irritation, so you need to assess the patient’s skin integrity. Some tubes also have 2 openings or attachments at the end. One of these openings is used solely for feeding and medication administration, while the other is used for flushing the tube.
Because each part of the tube can easily get dislodged or misplaced, nursing responsibilities are also included in ensuring that the equipment is complete and functioning as expected. The nurse should also remember that patients with PEG Tube require advance and rotation at least once every week to ensure the tube is appropriately placed and avoid the risk of developing a “buried bumper.” A buried bumper occurs when the bumper part of the tubing (the piece that attaches the tube into the stomach) embeds itself in the gastric mucosa.
Nursing care of the patient with PEG tube include, but are not limited to:
- Cleaning the stoma site
- Assessing patients for signs of complications of creating the stoma:
-
- Infection;
- Leakage of gastric acids;
- Inflammation; and
- Over-granulation.
-
- Ensuring the correct placement and non-migration of the tubing.
The RIG Tube
The RIG, or radiologically inserted gastrostomy tube, is an access site created and placed into the abdominal wall under the guidance of an x-ray. It is usually used for patients when:
- A PEG tube is not a viable option to be created, such as in patients with cancers that are at high risk of seeding or with respiratory complications;
- Patients cannot undergo endoscopic procedures such as issues in the anatomic structures of the pharynx;
- A previous unsuccessful PEG insertion attempt.
In the creation of a RIG, gastropexy is used to create the gastrostomy tract. The structure is then secured and supported in its place by skin fasteners and sutures along the abdominal wall. Several types of tubing are used in creating a RIG access site, but the same care performed for patients with PEG tubes is followed.
Nursing Care for Patients with PEG Tubes
Apart from ensuring that the tube remains in place and is free of infections, there are also other care requisites that you should remember in handling these patients. Below are the most common nursing considerations for patients with PEG tubes:
1. Provide patient education on how to clean the stoma site, especially since the tube will be inserted for the long term.
a. Observe sterile technique in cleaning the site initially, using sterile gloves, gauze, and saline until the area has healed.
b. Ensure that cleaning is done from the inside, going out to prevent the spread of infection.
c. Allow the site to dry, apply barrier film to protect the skin from the corrosive effects of gastric juices, and reposition the fixation plate
2. Observing advancing and rotating the tube to ensure proper placement:
Push the tube gently for at least 3-4cm into the abdomen until the tube is freely moving;
a. Gently pulling the tube back into the abdomen until resistance is felt.
b. Make sure that there is no associated discomfort in this process;
Securing the fixation plate into the abdomen once properly placed (the tip should be approximately 1cm from the skin to prevent ischemia).
3. Involving the patient and significant others during feedings and allowing them to demonstrate back what was learned during patient education.
4. Observe the patient for signs of complications and report them to the physician.
Health Education for Patient with PEG Tubes/RIG Tubes
Having PEG tubes created as access for feeding and medication bring about changes to the patient and family. It is important that you are able to educate the patient before the creation of the stoma. This would help ease some concerns about the risk of complications. Patients and Caregivers at home should be taught on:
- Identifying the signs and symptoms of infection, such as:
-
-
- Swelling and tenderness;
- Pain on the stoma site;
- Redness of the stoma and other changes in color;
- Pus formation and;
- Foul smell coming from the stoma.
-
- Noting for warning signs of PEG tube complications and when to refer to the situation to the physician:
-
- Dislodgement of the tube- cover the site with a sterile dressing and go to a hospital immediately
- Leakage around the tube- it may indicate wrong disc size or misalignment of the tube;
- Bleeding from the tube insertion site.
-
- First actions when the tube is accidentally displaced or pulled out;
- The activities that the patient can and cannot do while the PEG tube is in place:
-
- No contact sport
- Cover the tube and its surrounding area when swimming and perform stoma care immediately after swimming
- Yoga and other exercises that involve working on the abdominal muscles may be restricted
-
- Feeding schedules and procedure:
-
- Starting from clear liquids and progressing to full liquid slowly;
- How to administer feedings and medication through the tube.
-
- Potential complications of feeding:
-
- Diarrhea after feedings;
- Bloating and abdominal distention for more than 1 hour after feedings;
- Constipation or passing of dry and hard stools;
- Coughing or shortness of breath after feeding or medication administration;
- Regurgitation and tasting medication or feeding solution in the mouth after or between feedings.
-
It is also important to explain to the patient the need to use a sterile technique to clean the tube site during the first two weeks after being created. The following tips should be included in the teaching plan for tube care in the immediate postoperative period are:
- Observe proper handwashing and use sterile gloves when touching the stoma site.
- Avoid placing bulky or occlusive dressings over the operative site.
- Never place a gauze dressing under the disc. This can serve as a culture medium for the growth of microorganisms, which may lead to infections.
- Cleanse the site at least twice per day using a mild soap and water. If using soap is not feasible for some reason, sterile saline on cotton balls or swabs will do.
- Ensure that the site is cleansed gently. Never tug or pull at the skin near or surrounding the stoma.
- Dry the skin thoroughly before putting the disc back on.
- Never use ointments, creams, sprays, powders, or other preparation around the PEG tube and the stoma unless prescribed by the physician.
- Refrain from touching the tube or the site unless necessary.
See also
Conclusion
The main reason patients need PEG tubes or another form of enteral access devices is to ensure that the body gets all the nutrients, fluids, and medication it needs for a faster recovery. The nurse is the patient’s primary care provider in the initial stages, but in cases where the access sites are placed for long-term use, there is a need to involve the patient and their families in their care.
The nursing knowledge and skills needed for this type of care are more complex than the usual provision of nutrition to patients who can tolerate food orally and are therefore developed over time with training and experience. What is important is that safe and effective care is provided to the patient, and the risks of complications are managed well.
References
- O’Leary-Kelley, C. and Bawel-Brinkley, K., 2017. Nutrition Support Protocols: Enhancing Delivery of Enteral Nutrition. Critical Care Nurse, 37(2), pp.e15-e23.
- Roveron, G., Antonini, M., Barbierato, M., Calandrino, V., Canese, G., Chiurazzi, L., Coniglio, G., Gentini, G., Marchetti, M., Minucci, A., Nembrini, L., Neri, V., Trovato, P. and Ferrara, F., 2018. Clinical Practice Guidelines for the Nursing Management of Percutaneous Endoscopic Gastrostomy and Jejunostomy (PEG/PEJ) in Adult Patients. Journal of Wound, Ostomy and Continence Nursing, 45(4), pp.326-334.
- Dougherty, L. and Lister, S., 2011. The Royal Marsden Hospital Manual Of Clinical Nursing Procedures. Chichester, West Sussex: Wiley-Blackwell.
- Adeyinka A, Rouster AS, Valentine M. Enteric Feedings. [Updated 2020 Jul 28]. In:StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532876/
- Samuels LE (2019). Nasogastric and feeding tube placement. In: Roberts JR, Custalow CB, Thomsen TW, eds. Roberts and Hedges’ Clinical Procedures in Emergency Medicine and Acute Care. 7th ed. Philadelphia, PA: Elsevier.
- Twyman SL, Davis PW (2020). Percutaneous endoscopic gastrostomy placement and replacement. In: Fowler GC, ed. Pfenninger and Fowler’s Procedures for Primary Care. 4th ed. Philadelphia, PA: Elsevier.



![Caring for Patients with Tracheostomy and Nursing Diagnoses [ Updates] tracheostomynursingprocedure](https://rnspeak.com/wp-content/uploads/2020/10/tracheostomynursingprocedure_725820712-238x178.jpg)



