Blood transfusion is one of the most common interventions patients prescribed to receive, especially in cases of severe blood loss. Transfusions usually occur when a venous access is created to allow the patient to receive blood and blood products aimed to help restore adequate circulating blood volume. The most commonly transfused blood components are the red blood cells, followed by plasma and fresh whole blood. In cases where patients exhibit bleeding problems, clotting factors may also be transfused.
There are several conditions which may prompt a patient to receive a blood transfusion, such as:
- Anemia, which may be secondary to:
- Leukemia and other types of cancers;
- Liver failure/liver cirrhosis; and
- Renal failure;
- Bleeding disorders of pregnancy;
- Severe blood loss due to surgery; and
- Blood loss due to trauma, injury, or other medical conditions.
Transfused blood products can also be one or more of the following, depending on patient needs and the goals of care:
- Fresh whole blood (FWB) consists of all components in donated blood and transfused to the patient over a prescribed period of time. This is usually prescribed when an immediate increase in the total blood volume is needed.
- Packed red blood cells (PRBC)- Normally transfused no more than 4 hours per bag, this blood component is prescribed for patients who can only tolerate smaller volumes of blood transfusion. This component is usually transfused in series and recommended, especially when the patient needs an increase in the hematocrit count.
- Platelets- Mainly prescribed for patients who have bleeding problems, platelets are transfused as rapidly as the patient can tolerate it (over a period of 30 minutes to 1 hour). This is because most patients prescribed to receive platelet transfusions exhibit moderate to severe bleeding problems, and there is a need to stop the bleeding as soon as possible.
- Plasma; fresh frozen plasma (FFP)- The transfusion of plasma is generally recommended for patients who require volume expansion but do not need all the components of fresh whole blood. Plasma is also recommended to be administered rapidly because the coagulation factors contained in it become unstable once it reaches room temperature.
- Albumin- Recommended for patients with severe blood volume deficiency and hypovolemic shock, albumin is transfused to maintain colloidal osmotic pressure. This is also recommended for patients who are suffering from hypoalbuminemia.
- Granulocytes- This blood component is prescribed for patients who are suffering from infections and have granulocyte levels of 500/mm3 and below. The infusion of granulocytes works best for patients who do not respond very well to antibiotic therapies.
- Cryoprecipitate- This component is one of the more expensive ones to extract, process, and has limited supplies. Recommended for patients who have diseased such von Willebrand’s disease and Hemophilia A. It is also a treatment of choice for pregnant women who suffer from DIC or disseminated intravascular coagulation.
- Factor VIII and Factor IX Concentrates- Factor VIII is also known as Hemophilia Factor A while Factor IX is called Hemophilia Factor B. Both concentrates are used for the specific types of diseases they are named after and are prescribed to help control bleeding. However, because these factors are usually pooled from numerous donors, there is a risk of transmission of HIV, Hepatitis B, and other blood-borne infectious diseases from transfusing them.
Blood and Blood Groups
Blood and Its Components
Blood is the main fluid component in the body that transports nutrients and oxygen throughout the body. It has several components that perform specific functions, such as:
- Red Blood Cells- also called erythrocytes, is responsible for carrying oxygen and nutrients throughout the body. RBCs get charged with oxygen in the lungs, where it also releases the carbon dioxide it gathers from the cells and organs of the body. Carbon dioxide is released from the body through exhalation. There are 2 main components of RBC:
- Hemoglobin- the portion of RBC that contains iron, giving it the red color that blood is known for. It is responsible for transporting oxygen throughout the body.
- Hematocrit- Mainly a measure of the number of red blood cells compared to the total blood volume and cell count, hematocrit is measured in percentages. It is usually used to denote the hydration status of a patient.
- Plasma- This is the liquid portion of the blood and is comprised of protein molecules, fat, sugar, and water. Plasma also plays a role in transporting red blood cells and other components throughout the body as it also helps in eliminating waste products from the circulation. Plasma is also responsible for maintaining adequate fluid balance.
- White Blood Cells (WBC)- Functioning mainly to protect the body from infections, WBCs number fewer than red blood cells. White blood cells are further categorized as:
- Neutrophil- the main white blood cell component and is responsible for approximately 55% to 70% of all WBC actions. This component has a very short life span (less than 24 hours) and is created continuously by the bone marrow; hence transfusions of neutrophils are not recommended.
- T cells/ T lymphocytes are responsible for immediate immune response, T cells help maintain protection by directly attacking cells and tumors that are already infected.
- B cells/B lymphocytes are responsible for creating antibodies that target specific viruses, bacteria, and other foreign bodies.
- Platelets- These are small cellular fragments that are mainly responsible for coagulation. Platelets function by gathering at an injured site (or a site where bleeding occurs) and forms a matrix for the fibrin clot to assemble and cover the injured site, preventing leaking of blood. This means that the overproduction of platelets causes clotting problems and deficient levels of such leads to bleeding problems.
A deficiency in the total circulating blood volume or its components causes problems in a patient’s body functions. These include oxygenation, control of bleeding, and distribution of nutrients throughout the body. Anemia and hypovolemia are some of the most common problems in terms of blood volume and the presence of red blood cells in it.
Blood Groups
Blood transfusion requires that the nurse is aware of the blood type of the patient prior to placing an order for blood components. This is because there are specific antigens present in each blood type, which may be incompatible with others. When such happens, the blood transfusion may not be helpful for the patient and may even create other health problems.
Blood types are grouped according to the ABO system, which determines blood types based on the two antigens and two antibodies that are present in the blood. These are antigens A and B, and antibodies A and B. Below is a diagram explaining the 4 different blood types.
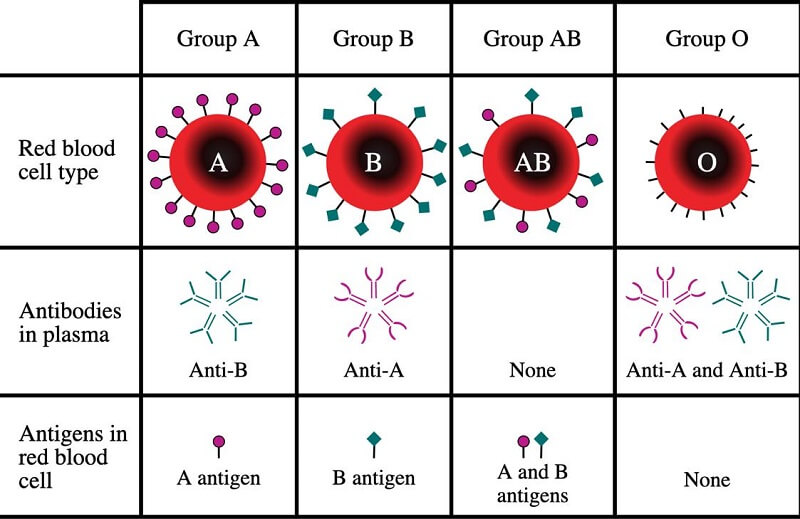
Apart from the ABO blood group, there is also the Rh System. This system is centered on the Rh (or Rhesus) presence factor, based on the D antigen present in the blood of an individual. This is denoted by the use of the + or – signs after the blood type, indicating the presence or absence of the D antigen. The Rh factor is especially important when it comes to crossmatching of blood samples to determine compatibility. Simply stated, a patient with Rh+ blood can be transfused with both Rh+ and Rh- blood, while a patient with Rh- blood can only receive Rh- blood.
Blood Components and Indications for Transfusion
- Packed RBCs. PRBCs are mainly recommended for patients with low erythrocyte or hemoglobin counts.
- 1 unit of PRBC is usually between 400-500mL and transfused over a period no longer than 4 hours.
- Effectiveness of intervention is determined through an increase in hemoglobin and hematocrit levels, taken within 4-6 hours after completing transfusion.
- It is indicated for patients with thrombocytopenia and other clotting problems.
- Fresh Frozen Plasma. FFPs can prescribe either to help increase circulating fluid volume or clotting factors.
- Should be transfused within 2 hours after thawing and run for 15 to 30 minutes once hooked.
- It is indicated for patients with sepsis or neutropenia. In some cases, this is also given to patients who do not respond to massive doses of antibiotics.
- Effectiveness of care may be evaluated through monitoring differential counts, and total WBC counts a few hours after transfusion.
- Cryoprecipitates and Others. Indicated for patients with deficiencies in clotting factors and fibrinogen, Hemophilia A and B.
- Each unit must be transfused for a period between 15-30 minutes.
- The effectiveness of therapy is evaluated through coagulation studies.
Blood Transfusion Nursing Responsibilities
Most blood transfusions happen in an inpatient setting, where a physician prescribes an individual to receive blood products to address an urgent health problem. When transfusing blood, the following must be remembered to help ensure safe and effective care for patients is maintained and provided:
- Ensure that the correct preparation of the patient and the care procedure is done.
- Double-check the order for transfusion and correlate this with the clinical diagnosis and care plan of the patient.
- Verify the blood type of the patient on the chart. If needed, obtain a request for blood typing.
- Once blood to be transfused or a donor is available, request for crossmatching to be done. A sample will be obtained from the patient and from the donor/blood pack and tested.
- After crossmatching is done, a request for the number of units to be transfused should be made.
- NOTE: Universal donor is blood type O-, while type AB+ is the universal recipient.
- Obtain consent. The consent must be obtained prior to starting any invasive procedure or therapy. NOTE: The physician is the one explaining the procedure and asks the patient to sign the form. The role of the nurse is to witness the signing.
- Assess for any allergies the client may have.
- Ask the client for any previous blood transfusion and their reaction to it.
- If the patient has had a BT before, the physician may need to prescribe premedication to prevent a febrile non-hemolytic reaction, common with patients who have had several blood transfusions done.
- Usual premedication given is Benadryl (diphenhydramine) and acetaminophen, 30 minutes to 1 hour before transfusion.
- Verify the BT order. Check the patient record and the order of the physician. The following are verified:
- Patient identification and the information about the patient from the blood bank;
- Results of typing and crossmatching;
- Expiration date of the blood product to be administered.
- Warm the blood products.
- Determine the correct gauges of IV needle. Usual IV needles from a blood transfusion are gauge 18 0r 16. Larger bore needles are needed for BT because it allows the passage of RBCs.
- Ensure proper IV tubing and access site. Y-tubing with an in-line filter is typically used for BT. If the patient needs any other IV fluids, this is administered on another line.
- Prime the line. The BT line is primed prior to the administration of BT. 0.9% NaCl is used to prime the line and is the only compatible IV fluid with blood transfusions. NOTE: Once the line is primed, the BT can be started.
- Obtain vital signs. These vital signs are taken prior to the start of the BT and several times during the BT. Blood pressure, temperature and pulse rate can be used as indicators of potential adverse reactions to transfusion.
- Start the transfusion. Ensure that the patient is positioned comfortably since the BT may last for anytime between 30 minutes to 4 hours.
- Monitor patient response to the therapy. Apart from vital signs, the patient may be assessed for the following:
- Rashes. This is an indication of an allergic reaction either to the blood type or the additives in the blood products.
- Chills. A sign of a pyrogenic reaction, especially when this is seen in the patient with an increase in temperature.
- Shortness of breath. This is a sign of hemolytic reaction and necessitates the stopping of the transfusion.
- Headache, back pain, nausea and vomiting.
- NOTE: If using an infusion pump, set the pump at 2mL/min for the first 15 to 30 minutes of transfusion and monitor the patient’s response. Vital signs must be monitored as per the following schedule:
- At the first 5 minutes after starting the transfusion;
- 15 minutes after transfusion started;
- On the 30th minute;
- Every hour until the transfusion is done;
- 1 hour after the transfusion is over.
- Once transfusion is done, the line should be flushed with normal saline solution. If there are no more succeeding transfusions, the line is discontinued, and the BT set is disposed of properly.
Transfusion Reactions
Blood transfusion reactions may occur anytime from the start of the transfusion until a few hours after the transfusion is done. The most common transfusion reactions include but are not limited to:
- This type of reaction occurs because the white blood cells of the patient react with the donor blood. This reaction causes the patient’s body to increase its production of antibodies, causing an increase in the body temperature from 1 to 1.8 degrees centigrade. In some cases, this is accompanied by chills, headaches, and an increase in the heart rate.
- An allergic reaction to the blood components and additives may not only cause allergies but also lead to anaphylaxis and is an emergency situation. Anaphylactic reactions are normally accompanied by hives, rashes, wheezes, and tightening of the airways.
- This reaction occurs because the patient’s immune system targets the red blood cells in the donor blood. This usually happens when blood transfusions are not properly typed and crossmatched. When this is not addressed correctly, this may lead the patient to exhibit:
- Renal failure;
- Disseminated intravascular coagulation (DIC);
- And in worse cases, death.
- Graft vs Host Disease. Also known as GvHD, this complication occurs a few days to a few weeks after the end of the transfusion. This happens because the T lymphocytes of the patient react to the blood transfused and are killed by the immune system.
- Other reactions.
- Septicemia
- Contamination of blood and blood products by HIV, Hepatitis B, and other blood-borne infections
- Circulatory overload (when the blood is transfused too rapidly, or in cases when patients have comorbid conditions such as congestive heart failure, kidney problems, etc.)
Stopping Blood Transfusions
Stopping a blood transfusion involves more than just discontinuing the line. Legal responsibilities of the nurse caring for patients undergoing blood transfusions include documenting the reaction of the patient, obtaining vital signs, following institutional protocols for such occurrence, and notifying the physician about the reaction of the patient. The following are the steps in stopping blood transfusions when a reaction occurs:
- Stop the flow of the transfusion and flush the line with 0.9% normal saline solution.
- If needed, the line must be disconnected from the set-up, and a new tubing must be used to ensure that the line is kept patent and no new insertions of the access site are to be made.
- Take the patient’s vital signs, document them together with all the reactions seen and complained by the patient.
- Notify the physician immediately of the event.
- Inform the blood bank of the event.
- Be prepared to administer medications to the patient to combat any reaction that must be addressed:
- Antihistamines
- Corticosteroids
- Vasopressors
- Epinephrine
- Diuretics
- Coordinate with the laboratory the need for tests and studies to rule out other complications.
- Save the blood bag and other related equipment for inspection and assessment if needed. Make sure that these are correctly labeled.
Conclusion
The nurse caring for a patient undergoing blood transfusion is expected to know the safe and effective care management of the patient. Apart from the need to ensure proper hemodynamic balance, the risk for complications is also managed well. Appropriate assessment, proper documentation, and knowing the history of the patient well are great help in ensuring that the patient will receive the right intervention.
References
- Basavanthappa, B., (2015). Medical-Surgical Nursing. New Delhi: Jaypee Brothers Medical Publishers.
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Hinkle, J.L. & Cheever, K.H. (2018). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (14th ed.). Philadelphia: Wolters Kluwer.
- Morton, P., & Fontaine, D. (2018). Critical Care Nursing. Wolters Kluwer.
- Potter, P.A., Perry, A.G., Stockert, P.A., & Hall, A.M. (2019). Essentials for Nursing Practice (9th ed.). St. Louis: Elsevier.



![Caring for Patients with Tracheostomy and Nursing Diagnoses [ Updates] tracheostomynursingprocedure](https://rnspeak.com/wp-content/uploads/2020/10/tracheostomynursingprocedure_725820712-238x178.jpg)




Dear madam; i appreciate your services, specialy for nurses.
Thank you for the added information
Some added info: look out for these keywords in your pts.
Itch/rash = allergic rxn
Itch/rash + respiratory involvement = anaphylaxis
Increase in temperature by 1 degree = febrile rxn
Flank/back pain = hemolytic rxn
In any case, remember SPINS:
S = stop infusion
P = pulses & vital signs should be monitored
I = infuse NSS using a different line in a different site. More blood would be infused (causing more damage) if you use the same line.
N = notify the doctor
S = samples of the first voided urine as soon as adverse reaction was noted (to check for renal function) and blood samples (to find out what’s going on)