Insulin, the medication of choice for patients, tends to work primarily in the body’s liver, muscles, and tissues. This allows it to bind to cellular receptors on membranes, facilitating the passage of glucose and electrolytes like potassium and magnesium. While the drug is initially prescribed for patients with Type 1 diabetes, it is also recommended for patients with Type 2 diabetes whose blood sugar levels cannot be adequately controlled with oral anti-diabetic drugs.
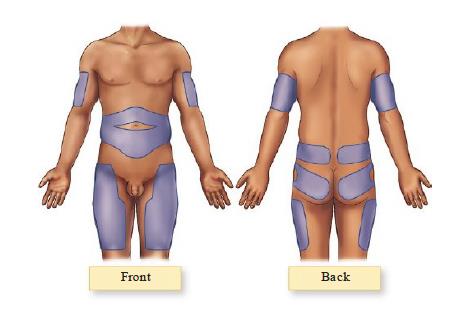
Due to the drug’s mechanism of action, it is often administered in the fatty areas of the body, such as the posterior surface of the arms, the anterior surface of the thighs, and the hips. However, the most common site of administration for most patients is on the abdominal area (see Figure 1). It is worth noting that the abdominal fat roll is the most commonly chosen site of insulin injection due to its ability to absorb the drug more rapidly and evenly than the other sites.
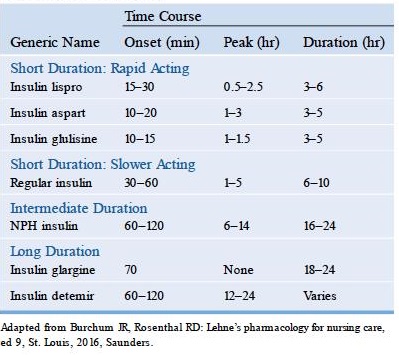
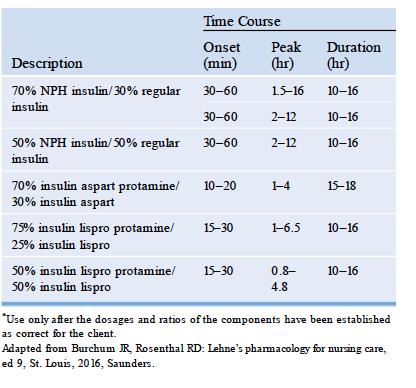
There are different drug mechanisms depending on the type of insulin. The onset of action varies from as short as 15-30 minutes to as long as 2 hours. The onset of action, peak, and duration of the action of insulin also varies depending on whether it is administered as a single or mixed type. In most cases, insulin injections composed of a mixture of short-acting and long-acting types of varying percentage compositions are shown to have a prolonged effect that those administered composed only of single doses.
The tables below show the average onset, peak and duration of action of insulin:
Injecting Insulin
In caring for patients who are receiving insulin injections, the nurse must remember the following reminders and/or patient teaching:
- Injection sites for insulin should be rotated systematically to avoid lipodystrophy and to help ensure optimal absorption.
- When rotating sites, it should be done in the same anatomical area; sites cannot be used more than once in a 2- to 3-week period.
- Sites for injections in the same anatomical area should be set at least 1 to 1.5 inches apart.
- It is not recommended that insulin injection sites be massaged, applied with a warm compress, and patients are encouraged to exercise to increase absorption. The patient must be cautioned that these activities and/or engaging in exercise may cause hypoglycemia.
- Ensure that when administering insulin, proper dosing must be followed.
Preparing Insulin Injections
The following are the tips and precautions to be observed in preparing insulin injections:
- Ensure that the insulin syringe to be used is calibrated to match the concentration of the drug in the vial. The usual concentration of insulin is expressed as U-100, which is equivalent to 100 units per mL of fluid.
- Remember that the Humulin R brand of insulin is formulated in U-500 strength and is usually reserved only for patients with severe insulin resistance. Use of this type of insulin requires a special syringe calibrated at a U-500 strength.
- Gauge 27 or 29 needles usually are used for insulin syringes. These needles are approximately ½ inch long.
- NPH insulin is the only type that comes as a suspension and appears cloudy. The rest are solutions and come out clear in appearance.
- When using NPH insulin, remember that the vial must be rolled between the palms or is rotated to help ensure that it is well-mixed.
- Gently roll the vial between the palms of the hands.
- Never shake the vial. This can cause air bubbles to form inside the liquid and lead to incorrect dosing.
- Inject air into the insulin vial prior to drawing it up. This helps relieve the vacuum inside the vial and makes it easier for the drug to be aspirated into the syringe.
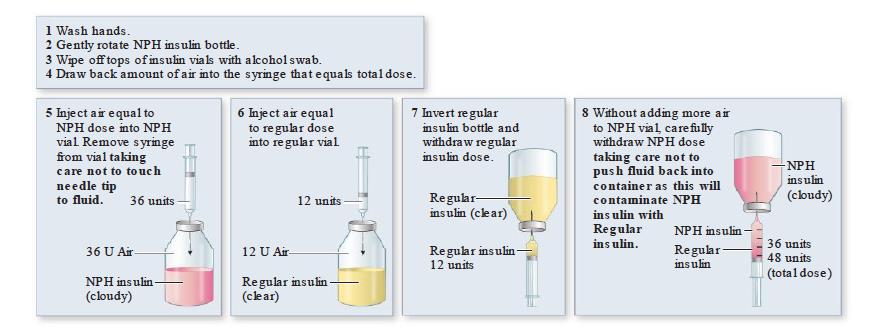
- When mixing insulin dosages in one syringe, draw up the shortest acting insulin first.
- Note that short-acting/short duration insulin preparations such as regular, lispro, apart, and gluisine can be mixed with NPH insulin.
- Insulin glargine cannot be mixed with any other type of insulin.
- Ensure that insulin is administered no more than 15 minutes after preparation. This ensures that the short-acting insulin does not bind with the NPH insulin, causing it to reduce its action.
- When self-injecting insulin, it is not generally recommended to aspirate after insertion of the needle.
- During the administration of the insulin, observe the following reminders:
-
- Use a 45- to 90-degree angle when injecting on a patient with normal subcutaneous tissue mass.
- For patients who are emaciated or with a decreased amount of subcutaneous mass, inject insulin observing a 45- to a 60-degree angle.
-
Because insulin is used as a replacement hormone, the nurse must remember that there are no definite contraindications to administering it. This means that insulin is a hormone that the body produces naturally, and exogenous insulin is used to help ensure that the hormone levels in the body are adequate. However, the nurse needs to pay special attention to pregnant or lactating patients because their needs differ from those of other patients. Special considerations must also be made when administering insulin to patients undergoing surgical procedures, those suffering from burns, or those experiencing extreme physical or emotional stress, as these can all affect insulin requirements.
Steps in Mixing insulins in One syringe
Example of Dose
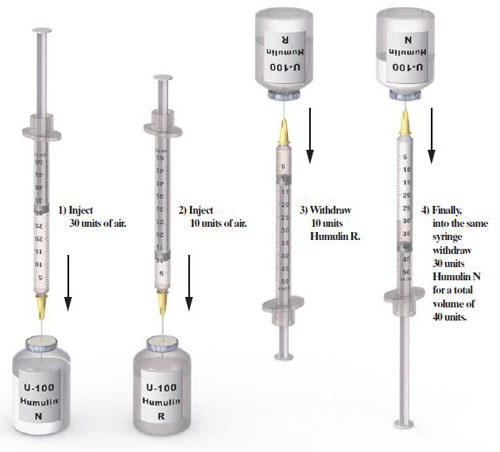
The doctor ordered 10 units of Humulin R insulin and 30 units of Humulin N insulin subcutaneously, 30 minutes before breakfast.
Since the doctor ordered two different insulin preparations to be mixed in the same syringe and your stock is not premixed. They need to be mixed manually in one syringe. Mixing insulin requires extra steps that must be completed in a specific order.
10 units of clear [ R(Regular) insulin]
+ 30 units of cloudy [N(NPH) insulin]
= 40 total units. [Total mixe dose]
To administer the dose, use 50 units of Lo-Dose syringe
How would you prepare to administer this injection?
Instructions:
- Gather all of the equipment you will need
- Wash your hands
- Check the expiration date on the vials of insulin. If they are not expired, pick up the cloudy insulin bottle and roll it between your hands until it is mixed, until there is no powder on the bottom of the bottle. Do not shake the insulin bottle because this can cause air bubbles.
- Take the bottle of cotton ball dipped in alcohol and wiped the top of both insulin vials.
- Pick the Humulin N (slower acting insulin) first and inject 30 units of air into the vial.
- After putting air in the Humulin N(slower acting insulin), do not draw up the insulin yet. Just pull the needle out and insert 10 units of air into the Humulin R( faster-acting insulin) vial.
- Then, after you inject the air into Humulin R (faster-acting insulin), turn the vial upside down to draw 10 units of Humulin R( faster-acting insulin) into the syringe.
- Once you have drawn up your 10 units, Insert the needle into the vial of Humulin N (slower-acting insulin) and draw the slower-acting insulin into the syringe (in this case,30 units for a total of 40 mixed-dose units into the syringe)
See Also
Nursing Care for Patients Having Insulin Injections
Administering insulin injections requires the nurse to be more careful, especially since apart from the need to calibrate doses, monitoring patient response to medication should be made. The following are nursing considerations for patients who are receiving insulin injections as part of their therapies for diabetes mellitus:
- Perform a thorough assessment on the potential for contraindications or any complications arising from insulin therapy such as pregnancy, history of allergies, and other premorbid conditions.
- Ensure that proper blood sugar monitoring is performed to help determine the need to adjust doses as needed.
- Determine the level of physical activity and independence that the patient exerts so that the plan of care and other treatment regimes may be modified or changed according to his needs.
- Monitor other laboratory values of the patient and involve him in planning for its monitoring, especially when the insulin therapy plans a long-term care management plan.
- Work with the patient to ensure that his diet and activity plans help enhance the increased effectiveness of insulin therapy.
- Provide teaching to the patient and his significant others the importance of following the recommended treatment regimen for the patient to prevent complications such as:
- Proper diet
- Adherence to medication regimen (dosages, time of taking medications, and proper route of administration)
- Activity and other lifestyle factors
- For breastfeeding and lactating women: remind them that insulin does not enter the breastmilk and would not have any effect on the infant. However, it may reduce milk production.
- Ensure that the proper steps for preparing insulin injections are observed and taught to patients and their significant others:
- Checking blood sugar levels prior to injecting
- Sliding the recommended dosage based on obtained blood glucose levels
- Injecting insulin at least 30 mins prior to mealtimes
- Caution the patient about mixing insulin types, especially when prescribed to aspirate them from different containers.
- Teach the patient proper storage of insulin to help maintain its potency and effectiveness.
- Vials should be placed away from direct sunlight. Some brands may require refrigeration.
- Pre-filled syringes must be refrigerated to help maintain stability.
- It is recommended that when transporting insulin, they are placed on a cold carrier or a tumbler filled with ice.
- When teaching patients to self-administer insulin, the nurse should include the following:
- Demonstrating the proper way of rolling the vials of insulin (if they are used)
- Maintaining proper rotation of insulin sites to prevent lipodystrophy
- Following aseptic technique in administering insulin.
- Avoid massaging the injection site.
- Regularly monitor blood sugar levels to determine the effectiveness of therapy.
- Teach the patient signs and symptoms of hypoglycemia:
- Cold, clammy skin
- Weakness
- Dizziness
- Hunger pangs
- Palpitations
- Reinforce instruction on proper diabetic foot care to prevent gangrene formation such as:
- Wearing snug-fitting shoes and cotton socks
- Changing socks daily
- Keeping the feet and toes dry
- Avoiding walking barefoot
- Trimming toenails straight across to avoid injuring the toes
- Visits to a podiatrist when needed.
Conclusion
Patients who have prescribed insulin as part of their diabetes care management must receive health education because they will most likely be on this therapy for the rest of their lives. The continuity of their treatment regimen is ensured, and the risk of developing complications is reduced by involving them in their care.
Furthermore, as patients are encouraged to participate in their care, learn proper insulin administration techniques, and protect their medication from sunlight and other elements, they are empowered to take control of their health. While diabetes is undoubtedly a chronic disease that patients must live with for the rest of their lives, this does not signify that they should always suffer from its complications.
Signs and symptoms of hypoglycemia and hyperglycemia should be monitored in insulin therapy patients, and their responses to therapy should be noted. Furthermore, the nurse caring for the patient should ensure that all steps and procedures in dosing and administering the medication to the patient are followed to help achieve blood sugar control and give the patient the most optimal level of functioning possible despite the diagnosis.
References
- Basavanthappa, B., (2015). Medical-Surgical Nursing. New Delhi: Jaypee Brothers Medical Publishers.
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Hinkle, J.L. & Cheever, K.H. (2018). Brunner & Suddarth’s Textbook of Medical-Surgical Nursing (14th ed.). Philadelphia: Wolters Kluwer.
- Morton, P., & Fontaine, D. (2018). Critical Care Nursing. Wolters Kluwer.
- Potter, P.A., Perry, A.G., Stockert, P.A., & Hall, A.M. (2019). Essentials for Nursing Practice (9th ed.). St. Louis: Elsevier.




![Caring for Patients with Tracheostomy and Nursing Diagnoses [ Updates] tracheostomynursingprocedure](https://rnspeak.com/wp-content/uploads/2020/10/tracheostomynursingprocedure_725820712-238x178.jpg)




very informative topic
Thank you Almera 🙂