Mortality from diarrhea is overall globally declining but remains high. Most estimates have diarrhea as the second cause of childhood mortality, with 18% of the 10.6 million yearly deaths in children younger than age 5 years.
Diarrhea is the reversal of the normal net of the absorptive status of water and electrolyte absorption to secretion. The augmented water content in the stools (above the normal value of approximately 10 ml/kg/day in the infant and young children, or 200 g/day in the teenager and adults) is due to an imbalance in the physiology of the small and large intestinal processes involved in the absorption of ions, substrates, and thus water .
Diarrhea is categorized into acute or chronic and infectious or non-infectious based on the duration and type of symptoms.
- Acute diarrhea. Acute diarrhea is defined as an episode lasting less than two weeks. Infection most commonly causes acute diarrhea, and the course is usually self-limited.
- Chronic diarrhea. Chronic diarrhea is defined as a duration lasting longer than two weeks and tends to be non-infectious. Common causes include malabsorption, inflammatory bowel disease, and medication side effects.
Although infectious agents are by far the most common cause of sporadic or endemic episodes of acute diarrhea, one should not dismiss other causes that can lead to the same presentation. Causes of diarrhea include the following:
- Infections such as enteric infections, food poisoning, and extraintestinal infections
- Drug-induced for drugs such as antibiotics, laxatives, magnesium-containing antacids, and opiates during withdrawal
- Food intolerances or allergies such as cow’s milk protein allergy, soy protein allergy, multiple food allergies, olestra, and methylxanthines
- Disorders of digestive/absorptive processes such as glucose-galactose malabsorption, sucrase-isomaltase deficiency, and late-onset (adult-type) hypolactasia resulting in lactose intolerance
- Chemotherapy or radiation-induced gastroenteritis
- Surgical conditions such as acute appendicitis and intussusception
- Vitamin deficiencies such as niacin deficiency and folate deficiency
- Vitamin toxicity such as vitamin C and niacin or vitamin B3
- Ingestion of heavy metals or toxins such as copper, tin, and zinc
- Ingestion of plants like hyacinths, daffodils, azalea, mistletoe, Amanita species, and mushrooms
The clinical presentation and course of diarrhea depend on its cause and on the host. Signs and symptoms may include the following:
- Dehydration (lethargy, depressed consciousness, sunken anterior fontanel, dry mucous membranes, sunken eyes, lack of tears, poor skin turgor, delayed capillary refill)
- Failure to thrive and malnutrition (reduced muscle/fat mass, peripheral edema)
- Abdominal pain or cramping
- Borborygmi
- Perianal erythema
Diarrhea
Diarrhea is the result of reduced water absorption by the bowel or increased water secretion. A majority of acute diarrheal cases are due to infectious etiology, which causes the secretory form of diarrhea. In this instance, the watery stool is the result of injury to the gut epithelium. Epithelial cells line the intestinal tract and facilitate the absorption of water, electrolytes, and other solutes. Infectious etiologies cause damage to the epithelial cells which leads to increased intestinal permeability. The damaged epithelial cells are unable to absorb water from the intestinal lumen leading to loose stool.
An essential aspect of diarrhea management is replenishing fluid and electrolyte loss. The following are nursing diagnoses associated with diarrhea.
- Diarrhea
- Risk for Deficient Fluid Volume
- Risk for Electrolyte Imbalance
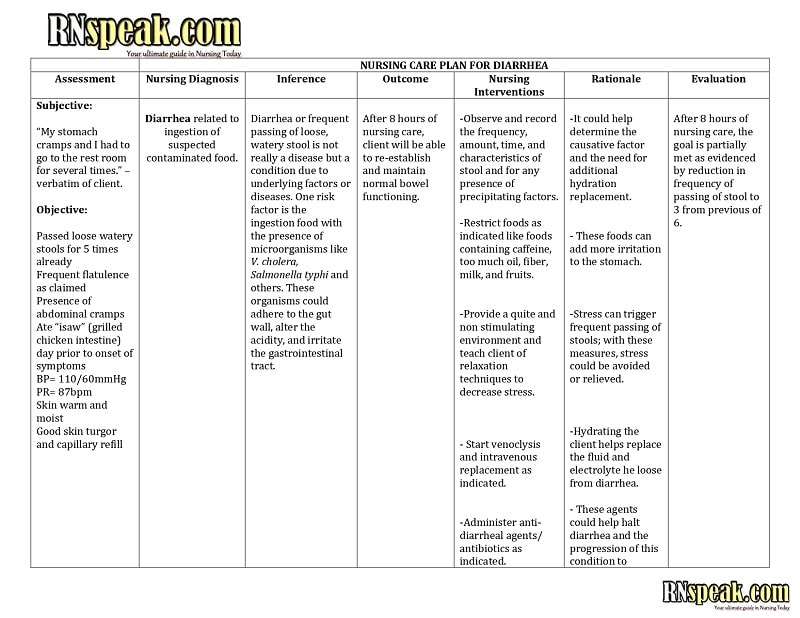
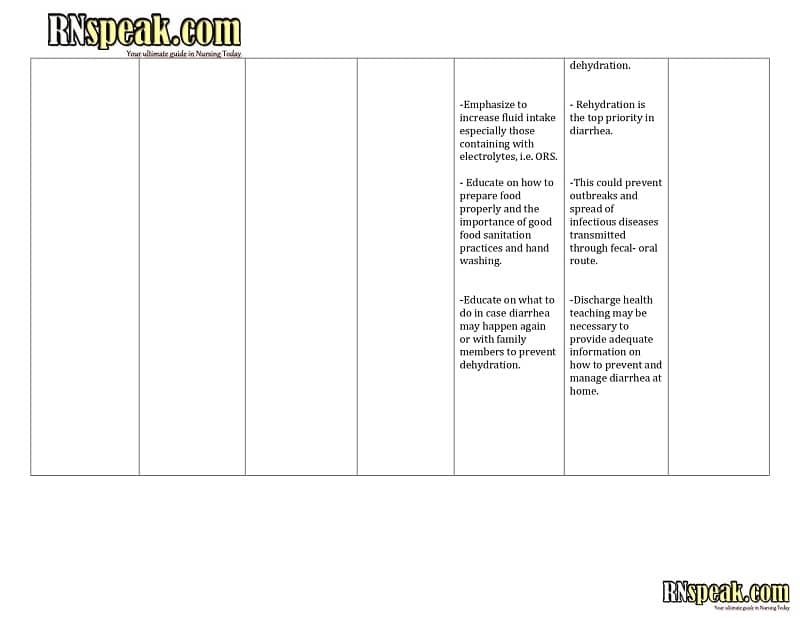
Diarrhea Nursing Care Plan
Below are sample nursing care plans for the problems identified above.
Diarrhea
Diarrhea is the augmentation of water content in stools because of an imbalance in the normal functioning of physiologic processes of the small and large intestines responsible for the absorption of various ions, other substrates, and consequently water. Such a derangement can be the result of either an osmotic force that acts in the lumen to drive water into the gut or the result of an active secretory state induced in the enterocytes. Diarrhea can also be osmolar in nature, as is observed after the ingestion of nonabsorbable sugars such as lactulose or lactose in lactose malabsorbers. Instead, in the typical active secretory state, enhanced anion secretion is best exemplified by enterotoxin-induced diarrhea.
Nursing Diagnosis
- Diarrhea
Related Factors
- Inflammation or irritation of the bowel
- Malabsoprtion
- Presence of toxins
- Segmental narrowing of the lumen
Evidenced by
- Increased bowel sounds, peristalsis
- Frequent, and often severe, watery stools
- Changes in stool color
- Abdominal pain; urgency, cramping
Desired Outcomes
- The client will report a reduction in the frequency of stools and return to more normal stool consistency.
- The client will identify and avoid contributing factors.
Nursing Interventions
| Assessment | Rationale |
| Observe and record stool frequency, characteristics, amount, and precipitating factors. | This helps differentiate individual diseases and assesses the severity of the episode. Knowledge of the characteristics of consistency, color, volume, and frequency can also be helpful in determining whether the source is from the small or large bowel. |
| Identify foods and fluids that precipitate diarrhea, such as raw vegetables and fruits, whole-grain cereals, condiments, carbonated drinks, and milk products. | Avoiding intestinal irritants promotes intestinal rest. Some foods may also contain organisms that can cause food poisonings such as Campylobacter and Salmonella species in dairy food and eggs . |
| Assess for fever, tachycardia, lethargy, leukocytosis, decreased serum protein, anxiety, and prostration. | These symptoms may signify that toxic megacolon or perforation and peritonitis are imminent or have occurred, necessitating immediate medical intervention. |
| Auscultate bowel sounds. | Postoperative paralytic or adynamic ileus usually resolves within 48 to 72 hours, and ileostomy should begin draining within 12 to 24 hours. Delay may indicate persistent ileus or sternal obstruction, which may occur postoperatively because of edema, improperly fitting pouch, prolapse, or stenosis. |
| Independent | |
| Promote bedrest and provide bedside commode. | Rest decreases intestinal motility and reduces the metabolic rate when infection or hemorrhage is a complication. Urge to defecate may occur without warning and be uncontrollable, thus increasing the risk of incontinence and falls if facilities are not close at hand. |
| Remove stool promptly. Provide room deodorizers. | This reduces noxious odors to avoid undue client embarrassment. |
| Encourage increased fluid intake gradually. Offer clear liquids hourly and avoid cold fluids. | This provides colon rest by omitting or decreasing the stimulus of foods and fluids. Gradual resumption of liquids may prevent cramping and recurrence of diarrhea; however, cold fluids can increase intestinal motility. |
| Encourage a diet high in fiber and bulk within dietary limitations. | This increases the consistency of the effluent. Although fluids are necessary for optimal body function, excessive amounts contribute to diarrhea. Breastfed infants with acute diarrhea should be continued on breast milk without any need for interruption. |
| Provide an opportunity to vent frustrations related to the disease process. | The presence of a disease, especially if the cause is unknown or is difficult to cure and may require surgical intervention, may lead to stress reactions that may aggravate the condition. |
| Assist with frequent perianal care. | Anal irritation, excoriation, and pruritus occur because of diarrhea. The client often cannot reach the area for proper cleansing and may be embarrassed to ask for help. |
| Dependent/Collaborative | |
| Administer antidiarrheal medications as indicated. | Antidiarrheal agents decrease GI motility or propulsion and diminish digestive secretions to relieve cramping and diarrhea. However, use these drugs with caution because they may precipitate toxic megacolon. |
| Administer anti-inflammatories such as mesalamine, sulfasalazine, and aminosalicylates. | Most people with mild or moderate ulcerative colitis are treated first with a group of drugs containing mesalamine, a substance that helps control inflammation. Sulfasalazine is the most commonly used of these drugs. Clients who do not benefit from it or who cannot tolerate it may receive aminosalicylic agents, which are given orally, through an enema, or in a suppository, depending on the location of the inflammation in the colon. |
| Administer anti-infectives such as metronidazole and ciprofloxacin. | These are used to treat bacterial overgrowth in the small intestine caused by stricture, fistulas, or prior surgery. This may be part of a long-term treatment regimen. |
| Administer steroids as prescribed. | Steroids decrease acute inflammatory processes. Steroid enemas may be given in mild to moderate disease to aid absorption of the drug- possibly with atropine sulfate or belladonna suppository. Current research suggests an 8-week course of time-release steroids may affect remission in Crohn’s disease; however, steroids are contraindicated if intra-abdominal abscesses are suspected. |
Risk for Deficient Fluid Volume
The negative fluid balance that causes dehydration results from decreased intake, increased gastrointestinal output, or fluid shift. The decrease in total body water causes reductions in both the intracellular and extracellular fluid volumes. Clinical manifestations of dehydration are most closely related to intravascular volume depletion and the physiologic compensation attempts that take place.
Nursing Diagnosis
- Risk for Deficient Fluid Volume
Risk Factors
- Excessive losses due to severe frequent diarrhea
- Inflammation, fever
- Restricted intake
- Chronic, excessive laxative use
Evidenced by
- [Not applicable; the presence of signs and symptoms establishes an actual diagnosis]
Desired Outcomes
- The client will maintain adequate fluid volume as evidenced by moist mucous membranes, good skin turgor, and capillary refill; stable vital signs; and balanced intake and output with normal urine concentration and amount.
- The client will verbalize understanding of causative factors and behaviors necessary to correct the fluid deficit.
Nursing Interventions
| Assessment | Rationale |
| Monitor intake and output. Measure urinary output and specific gravity | This provides information about overall fluid balance, renal function, and bowel disease control, as well as guidelines for fluid replacement. Increased specific gravity and decreased urine output reflect alterations in the circulating volume. |
| Assess vital signs such as blood pressure, pulse, and temperature. | Hypotension, including postural, tachycardia, and fever can indicate a response to and effect of fluid loss. |
| Note the number, character, and amount of stools. | In osmotic diarrhea, stool output is proportional to the intake of the unabsorbable substrate and is usually not massive. Flatulence associated with foul-smelling stools that float suggests fat malabsorption. |
| Evaluate skin turgor, capillary refill, and mucous membranes. | This reflects hydration status and the possible need for fluid replacement. Literature reviews have suggested that delayed capillary refill and delayed skin turgor are the most reliable clinical signs of dehydration in children. |
| Weigh daily. | Weight is another indicator of overall fluid and nutritional status. |
| Independent | |
| Provide clear liquids in small amounts when oral intake is resumed, and progress diet as tolerated. | This reduces the risk of gastric irritation and vomiting to minimize fluid loss. A strong body of evidence now suggests that resuming the prediarrhea diet is perfectly safe and must be encouraged, respecting any ) usually temporary) lack of appetite. |
| Provide oral rehydration solutions. | Rapid oral rehydration with the appropriate solution has been shown to be as effective as intravenous fluid therapy in restoring intravascular volume and correcting acidosis. ORS contains 2 to 3 g/dl of glucose, 45 to 90 mEq/L of sodium, 30 mEq/L of base, and 20 to 25 mEq/L of potassium. |
| Make fluids easily accessible to the client. Encourage the use of fluids that are tolerable to the client and that replace needed electrolytes, such as Gatorade and broth. | This enhances fluid intake. Certain fluids such as acidic fruit juices or iced beverages may be painful to consume due to cracked lips. |
| Give frequent mouth care with special attention to the protection of the lips. | Dehydration results in drying and painful cracking of the lips and mouth. |
| Dependent/Collaborative | |
| Administer intravenous fluids and electrolytes, as prescribed. | The peritoneum reacts to irritation and infection by producing large amounts of intestinal fluid, pulling fluid from the vascular space, and possibly reducing the circulating blood volume, resulting in dehydration and relative electrolyte imbalances. IV fluids are mostly indicated as rehydration therapy for severe dehydration, with intravenous lactated Ringer solution or normal saline. |
| Assist in the insertion of a nasogastric tube, as indicated. | If the client is unable to drink, administer through a nasogastric tube. |
| Avoid the administration of anti-motility agents as much as possible. | Antimotility agents are not indicated for infectious diarrhea, except for refractory cases of Cryptosporidium infection. |
Risk for Electrolyte Imbalance
The presentation of uncomplicated diarrhea in children is usually by the increased frequency and altered consistency of stools. In many cases, this is also accompanied by vomiting and abdominal pain. If appropriate treatment is not instituted, these clients may develop complications secondary to dehydration such as hypovolemic shock and renal failure. In some clients, electrolyte imbalance may occur leading to neurological manifestations such as lethargy or irritability and convulsions. The common electrolyte imbalances seen in clients with diarrhea include hypokalemia, hyponatremia, and altered urea and creatinine.
Nursing Diagnosis
- Risk for Electrolyte Imbalance
Risk Factors
- Diarrhea
- Drug-induced side effects
- Fever
- Treatment-related side effects
Evidenced by
- [Not applicable; the presence of signs and symptoms establishes an actual diagnosis]
Desired Outcomes
- The client will display heart rate, BP, and laboratory results within normal limits for the client.
- The client will exhibit an absence of muscle weakness and neurological irritability.
Nursing Interventions
| Assessment | Rationale |
| Monitor BP. | Either hypertension or hypotension may be present depending on the fluid status. The presence of postural hypotension may affect activity tolerance. |
| Monitor heart rate and rhythm. | Changes associated with hypokalemia include abnormalities in both conduction and contractility. Tachycardia may develop as well as potentially life-threatening atrial and ventricular dysrhythmias. |
| Note respiratory rate and depth. | Early identification and intervention prevent serious complications associated with this problem. |
| Monitor intake and output and urine specific gravity. Weigh daily. | These parameters are variable, depending on fluid status, and are indicators of therapy needs and effectiveness. |
| Assess the level of consciousness. | Sodium imbalance may cause changes that vary from confusion and irritability to seizures and coma. In the presence of a water deficit, rapid rehydration may cause cerebral edema. |
| Auscultate bowel sounds, noting absence or change, | Paralytic ileus commonly follows gastric losses through protracted diarrhea. |
| Assess skin turgor, color, temperature, and mucous membrane moisture. | Water-deficit hyponatremia manifests by signs of dehydration. |
| Independent | |
| Maintain safety and seizure precautions, as indicated, such as a bed in a low position and the use of padded side rails. | Sodium excess and cerebral edema increase the risk of convulsions. |
| Provide and encourage meticulous skin care and frequent repositioning. | This maintains skin integrity. |
| Provide frequent oral care. Avoid the use of mouthwash that contains alcohol. | Oral hygiene provides comfort and prevents further drying of mucous membranes. |
| Offer fluids at regular intervals. | This may prevent hypernatremia in a client who is unable to perceive or respond to thirst. |
| Recommend avoidance of foods high in sodium such as canned soup and vegetables, processed foods, snack foods, and condiments. | Avoidance of these foods reduces the risk of sodium-associated complications. |
| Encourage foods high in potassium such as bananas, oranges, dried fruits, red meat, leafy vegetables, and potatoes. | Potassium may be replaced and level maintained through the diet when the client is allowed oral food and fluids. Dietary replacement of 40 to 60 mEq/L is typically sufficient if no abnormal losses are occurring. |
| Discuss preventable causes of the condition such as nutritional choices and proper use of laxatives. | This provides an opportunity for the client to prevent a recurrence. Also, dietary control is more palatable than oral replacement medications. |
| Dependent/Collaborative | |
| Monitor serum electrolytes, osmolality, and arterial blood gasses, as indicated. | This evaluates therapy needs and effectiveness. However, co-occurring hyperchloremia may cause metabolic acidosis, requiring further intervention. Potassium levels should be checked frequently during replacement therapy. |
| Administer intravenous fluids as prescribed. Monitor the rate of IV potassium administration. | Replacement of total body water deficit will gradually restore sodium and water balance. Potassium is lost during diarrhea. When IV potassium is prescribed, use an infusion pump to ensure controlled delivery of medication to prevent the bolus effect and reduce associated discomfort. |
| Restrict sodium intake. | Restriction of sodium intake while promoting renal clearance lowers serum sodium levels in the presence of extracellular fluid excess. |
| Administer oral or IV potassium. | This may be required to correct deficiencies when changes in medication, therapy, and/or dietary intake are insufficient. Dietary supplementation may be used to produce a gradual equilibration if the client is unable to take oral food and fluids. |
Diarrhea Nursing Care Plan Sample
References
- Gopchade, A. (2019, September). Electrolyte Disturbances in Children Presenting with Acute Diarrhea: A Prospective Cohort Study. Journal of Medical Science and Clinical Research, 7(9). https://dx.doi.org/10.18535/jmscr/v7i9.136
- Guandalini, S., & Cuffari, C. (2020, January 31). Diarrhea: Practice Essentials, Background, Pathophysiology. Medscape Reference. Retrieved January 5, 2023, from https://emedicine.medscape.com/article/928598-overview#a1
- Huang, L. H., & Corden, T. E. (2018, December 7). Dehydration: Background, Pathophysiology, Etiology. Medscape Reference. Retrieved January 5, 2023, from https://emedicine.medscape.com/article/906999-overview#a5
- Murr, A. C., Doenges, M. E., & Moorhouse, M. F. (2010). Nursing Care Plans: Guidelines for Individualizing Client Care Across the Life Span. F.A. Davis Company.
- Nemeth, V., & Pfleghaar, N. (2022, November 21). Diarrhea – StatPearls – NCBI Bookshelf. NCBI. Retrieved January 5, 2023, from https://www.ncbi.nlm.nih.gov/books/NBK448082/