1. a, b, d, e
Rationale: PN is indicated in clients whose gastrointestinal tracts are not functional or must be rested, cannot take in a diet enterally for extended periods, or have increased metabolic need. Examples of these conditions include those clients with burns, exacerbation of Crohn’s disease, and persistent nausea and vomiting due to chemotherapy. Other clients would be those who have had extensive surgery, have multiple fractures, are septic, or have advanced cancer or acquired immunodeficiency syndrome. The client with the open cholecystectomy is not a candidate because this client would resume a regular diet within a few days following surgery.
Test-Taking Strategy: Note the strategic words, most likely, which tell the nurse that the correct options are the clients who require this type of nutritional support. Use nursing knowledge of these various conditions in the options and baseline knowledge
of the purposes of PN to make the selection.
Review: Parenteral nutrition
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Critical Care—Parenteral Nutrition
Priority Concepts: Clinical Judgment; Nutrition
Reference: Perry, Potter, Ostendorf (2014), p. 797.
2. 375
Rationale: If the IV is scheduled to run over 8 hours, the hourly rate is 125 mL/hour. Using 500 mL as the reference point, the next hourly marking would
be at 375 mL, which is 125 mL less than 500.
Test-Taking Strategy: Focus on the subject, intravenous infusion calculations. Use basic principles related to dosage calculation and IV administration to answer this question. Subtract 125 from 500 to yield 375.
Review: Administration of in tr aven ous medication s
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamental of Care—Medication/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter, Ostendorf (2014), pp. 710-711.
3. 2, 3, 4
Rationale: An infiltrated intravenous (IV) line is one that has dislodged from the vein and is lying in subcutaneous tissue. Pallor, coolness, edema, pain, numbness, and blanched skin are the results of IV fluid being deposited in the subcutaneous tissue. When the pressure in the tissues exceeds the pressure in the tubing, the flow of the IV solution will stop, and if an electronic pump is being used, it will alarm. Erythema can be associated with infection, phlebitis, or thrombosis. Formation of a red streak and purulent drainage is associated with phlebitis and infection.
Test-Taking Strategy: Focus on the subject, clinical manifestations at the IV site. Remember that pallor, coolness, pain, numbness, and swelling are signs of infiltration, and that infection, phlebitis, and thrombosis are associated with warmth at the IV site.
Review: Signs of infiltration
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Critical Care—Medications and Intravenous Therapy
Priority Concepts: Clinical Judgment; Tissue Integrity
Reference: Ignatavicius, Workman (2016), p. 204.
4. 1
Rationale: Clients who have undergone crainotomy should have the head of the bed elevated 30 to 45 degrees to promote venous drainage from the head. The client is positioned to avoid extreme hip or neck flexion and the head is maintained in a midline neutral position. The client should not be positioned on the site that was operated on, especially if the bone flap was removed, because the brain has no bony covering on the affected site. A flat position or Trendelenburg’s position would increase intracranial pressure. A reverse Trendelenburg’s position would not be helpful and may be uncomfortable for the client.
Test-Taking Strategy: Focus on the subject, positioning following craniotomy. Remember that a primary concern is the risk for increased intracranial pressure. Therefore, use concepts related to gravity and preventing edema and increased intracranial pressure to answer this question.
Review: Positioning following craniotomy
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Safety
Priority Concepts: Intracranial Regulation; Safety
Reference: Ignatavicius, Workman (2016), p. 960.
5. a, b, c, e
Rationale: By aspirating stomach contents, the residual volume can be determined and the pH checked. A pH less than 3.5 verifies gastric placement. The suction should be turned off before the tubing is disconnected to check for residual volume; in addition, suction should remain off for 30 to 60 minutes following medication administration to allow for medication absorption. There is no need to remove the tube and place it in the other nostril in order to administer a feeding; in fact, this is an invasive procedure and is unnecessary.
Test-Taking Strategy: Focus on the subject, instilling medication into the nasogastric tube, and visualize the procedure when answering this question. Read each option carefully and eliminate option 4 because it is not necessary and is an invasive procedure.
Review: Medication administration via a nasogastric tube
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Skills
Priority Concepts: Clinical Judgment; Safety
Reference: Perry, Potter, Ostendorf (2014), pp. 502, 786-788.
6. b, c, d, f
Rationale: Kohlberg’s theory states that individuals move through stages of development in a sequential fashion but that not everyone reaches stages 5 and 6 in his or her development of personal morality. The theory provides a framework for understanding how individuals determine a moral code to guide their behavior. It states that moral development progresses in relationship to cognitive development and that a person’s ability to make moral judgments develops over a period of time. In stage 1, ages 2 to 3 years (punishment-obedience orientation), children cannot reason as mature members of society. In stage 2, ages 4 to 7 years (instrumental-relativist orientation), the child conforms to rules to obtain rewards or have favors returned.
Test-Taking Strategy: Read each option carefully. Recalling that the theory provides a framework for understanding how individuals determine a moral code to guide their behavior and recalling the ages associated with each stage will assist in answering the question. Also noting the closed-ended word all in option 1 and the word mature in option 5 will assist in eliminating these options.
Review: Kohlberg’s theory of moral development
Level of Cognitive Ability: Applying
Client Needs: Health Promotion and Maintenance
Integrated Process: Teaching and Learning
Content Area: Developmental Stages—Infancy to Adolescence
Priority Concepts: Client Education; Development
Reference: Hockenberry, Wilson (2015), pp. 526, 575.
7. b, c, d, e
Rationale: Rubella vaccine is administered to women who have not had rubella or women who are not serologically immune. The vaccine may be administered in the immediate postpartum period to prevent the possibility of contracting rubella in future pregnancies. The live attenuated rubella virus is not communicable in breast milk; breast feeding does not need to be stopped. The client is counseled not to become pregnant for 1 to 3 months after immunization or as specified by the health care provider because of a possible risk to a fetus from the live virus vaccine; the client must be using effective birth control at the time of the immunization. The client should avoid contact with immunosuppressed individuals because of their low immunity toward live viruses and because the virus is shed in the urine and other body fluids. The vaccine is administered by the subcutaneous route. A hypersensitivity reaction can occur if the client has an allergy to eggs because the vaccine is made from duck eggs. There is no useful or necessary reason for covering the area of the injection with a sterile gauze.
Test-Taking Strategy: Focus on the subject, client instructions regarding the rubella vaccine. Recalling that the rubella vaccine is a live virus vaccine will assist in selecting options 2 and 5. Next, recalling the route of administration and the contraindications
associated with its use will assist in selecting options 3 and 4.
Review: Client instructions regarding the rubella vaccine
Level of Cognitive Ability: Analyzing
Client Needs: Health Promotion and Maintenance
Integrated Process: Teaching and Learning
Content Area: Maternity—Postpartum
Priority Concepts: Client Education; Immunity
Reference: Lowdermilk et al. (2016), p. 493.
8. c
Rationale: Station is the measurement of the progress of descent in centimeters above or below the midplane from the presenting part to the ischial spine. It is measured in centimeters and noted as a negative number above the line and as a positive number below the line. At the negative 1 (–1) station, the fetal presenting part is 1 cm above the ischial spine. Option 1 is at the negative 5 (–5) station and the fetal presenting part is 5 cm above the ischial spine. Option 2 is at the negative 2 (–2) station and the fetal presenting part is 2 cm above the ischial spine. Option 4 is at the positive 3 (+3) and the fetal presenting part is 3 cm below the ischial spine.
Test-Taking Strategy: Recalling that station is measured in centimeters and uses the ischial spine as a reference point will assist in answering this question. Focus on the data in the question and note the location of the ischial spine, and that the stations range from –5 cm to +5 cm above or below this reference point.
Review: Stations of the presenting part
Level of Cognitive Ability: Analyzing
Client Needs: Health Promotion and Maintenance
Integrated Process: Nursing Process—Assessment
Content Area: Maternity—Intrapartum
Priority Concepts: Clinical Judgment; Reproduction
Reference: Lowdermilk et al. (2016), p. 370.
9. c
Rationale: A patent ductus arteriosus is failure of the fetal ductus arteriosus (artery connecting the aorta and the pulmonary artery) to close. A characteristic machinery-like murmur is present, and the infant may show signs of heart failure. Aortic stenosis is a narrowing or stricture of the aortic valve. Atrial septal defect is an abnormal opening between the atria. Ventricular septal defect is an abnormal opening between the right and left ventricles.
Test-Taking Strategy: Focus on the subject, the congenital cardiac anomaly and the location of the defect. Recalling the anatomical locations in the heart will direct you to the correct option.
Review: Congenital heart defects
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Pediatrics—Cardiovascular
Priority Concepts: Clinical Judgment; Perfusion
Reference: Hockenberry, Wilson (2015), p. 1278.
10. b
Rationale: A bicornate uterus has a “Y” shape and appears to be a double uterus but in fact has only one cervix. A septate uterus contains a septum that extends from the fundus to the cervix, thus dividing the uterus into two separate compartments. A double uterus has two uteri, each of which has a cervix. A uterus didelphys occurs when both uteri of a double uterus are fully formed.
Test-Taking Strategy: Focus on the subject, the normal anatomy and appearance of the female reproductive organ.
Review: Anatomy of the female reproductive system
Level of Cognitive Ability: Recall and recognition
Integrated Process: Assessment
Content Area: Maternity Nursing
Priority Concept: Clinical Judgment; Assessment
Reference: Lowdermilk et al. (2016), p.
11. c, e
Rationale: The general contraindications for receiving live virus vaccines include a previous anaphylactic reaction to a vaccine or a component of a vaccine. In addition, live virus vaccines generally are not administered to individuals with a severely deficient immune system, individuals with a severe sensitivity to gelatin, or pregnant women. A vaccine is administered with caution to an individual with a moderate or severe acute illness, with or without fever. Options 1, 3, 4, and 6 are not contraindications to receiving a vaccine.
Test-Taking Strategy: Focus on the subject, contraindications for a live virus vaccine. This indicates that you need to select the situations in which a live virus vaccine cannot be given because doing so can cause harm to the child. Noting the word anaphylactic in option 2 and the words severely deficient in option 5 will direct you to these options.
Review: Contraindications to receiving a live virus vaccine
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Pediatrics—Infectious and Communicable Diseases
Priority Concepts: Clinical Judgment; Safety
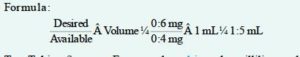
12. 1.5 mL
Rationale: Use the formula for calculating the medication:
Test-Taking Strategy: Focus on the subject, the milliliters to be administered. Note that the medication label indicates that there is 0.4 mg/mL. Use the formula to determine the correct dose, and verify the answer using a calculator.
Review: Medication administration guidelines
Level of Cognitive Ability: Applying
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Fundamentals of Care—Medications/IV Calculations
Priority Concepts: Clinical Judgment; Safety
Reference: Perry et al. (2014), pp. 485-487.
13. Rationale: Epidural anesthesia for a cesarean birth must be at the level of T4 to T6, approximately the nipple line. The level of anesthesia achieved via epidural
anesthesia for a vaginal birth is T10 (approximately the hips).
Test-Taking Strategy: Focus on the subject, the normal anatomy and appearance of the gravid patient.
Review: Anatomy; Anesthesia in labor and delivery
Level of Cognitive Ability: Recall and recognition
Integrated Process: Assessment
Content Area: Maternity Nursing
Priority Concept: Clinical Judgment; Assessment
Reference: Lowdermilk et al. (2016), p.
14. c
Rationale: The third maneuver involves grasping the lower portion of the abdomen just above the symphysis pubis between the thumb and index finger. This maneuver determines whether the fetal presenting part is engaged. The first maneuver involves facing the woman’s head and using the tips of the fingers to palpate the uterine fundus. This maneuver is used to identify the part of the fetus that lies over the inlet to the pelvis. The second maneuver involves placing the palms of each hand on either side of the abdomen to locate the back of the fetus. The fourth maneuver involves placing fingers on both sides of the uterus and pressing downward and inward in the direction of the birth canal. This maneuver is done to determine fetal attitude and degree of extension and should only be done if the fetus is in the cephalic presentation.
Test-Taking Strategy: Focus on the subject, the location of fundal height. Remember that during the second and third trimesters (weeks 18 to 30), fundal height in centimeters approximately equals the fetus’s age in weeks +/-2 cm.
Review: Measurement of fundal height
Level of Cognitive Ability: Analyzing
Client Needs: Health Promotion and Maintenance
Integrated Process: Nursing Process—Assessment
Content Area: Maternity—Antepartum
Priority Concepts: Development; Reproduction
References: Lowdermilk et al. (2016), pp. 287, 315-319.
15. 4, 2, 3, 1, 5.
Rationale: The nurse should immediately ask the client what her reaction is as a result of the exposure to Betadine. This gives the nurse an idea of whether there needs to be preparation for an event as severe as cardiac arrest or as simple as skin irritation. The nurse should then clean the Betadine from the client, notify the physician of the incident, and ask for an order for medication if needed to counteract the Betadine. The nurse will need to document the incident on the client’s chart as soon as the client has physically been taken care of. The nurse also will need to file an incident report.
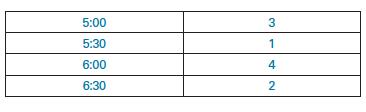
16. (see table below)
Rationale: Drawing the bilirubin levels at 6 a.m. must occur at a specific time. The admission assessment should be completed as soon after admission as possible; 5 a.m. is available to complete this task. The IV should be started at 6:30 and completed as close to change of shift as possible. The nurse should then draw the blood at 5:30 a.m., right after the newborn assessment.
17. 3, 5
Rationale: The nurses who have not had chickenpox or did not receive the varicella-zoster vaccine are susceptible to the herpes zoster virus and should not be assigned to care for the client with herpes zoster. Nurses who have not contracted roseola, mumps, or rubella are not necessarily susceptible to herpes
zoster. Herpes zoster (shingles) is caused by a reactivation of the varicella-zoster virus, the causative virus of chickenpox. Individuals who have not been exposed to the varicella-zoster virus or who did not receive the varicella-zoster vaccine are susceptible to chickenpox. Health care workers who are unsure of their immune status should have varicella titers done before exposure to a person with herpes zoster.
Test-Taking Strategy: Focus on the subject, transmission of herpes zoster. Recalling that herpes zoster is caused by a reactivation of the varicella-zoster virus, the causative virus of chickenpox, will direct you to the correct options.
Review: The relationship between herpes zoster and chickenpox
Level of Cognitive Ability: Analyzing
Client Needs: Safe and Effective Care Environment
Integrated Process: Nursing Process—Planning
Content Area: Leadership/Management—Delegating
Priority Concepts: Infection; Safety
Reference: Ignatavicius, Workman (2016), p. 451.
18. Answer: 240 calories.
Rationale:
45 mL = 10 oz
10 oz x 8 feedings = 12
12 x 20 calories/oz = 240 calories
19. Answer: 1
Rationale: In a neonate, the lateral aspect of the heel is the most appropriate site for obtaining a blood specimen. Using this area prevents damage to the calcaneus bone, which is located in the middle of the heel. The middle of the heel is to be avoided because of the increased risk for damaging the calcaneus bone located there. The middle of the foot contains the medial plantar nerve and the medial plantar artery, which could be injured if this site is selected. Using the base of the big toe as the site for specimen collection would cause a great deal of discomfort for the neonate; therefore, it is not the preferred site.
Test-Taking Strategy: Visualize how the intervention is to be performed, considering what is safe to do for the patient always.
Review: Anatomy of the foot of an infant
Level of Cognitive Ability: Applying
Client Needs: Safe and Effective Care Environment
Integrated Process: Nursing Process—Planning
Content Area: Development; Neonatal Care
Priority Concepts: Safety
Reference: Ignatavicius, Workman (2016), p. 451.
20. 1
Rationale: When assessing the incurving of the trunk tests for automatic refl exes in the newborn, the nurse places the infant horizontally and in a prone position with one hand, and strokes the side of the newborn’s trunk from the shoulder to the buttocks using the other hand. If the reflex is present, the newborn’s trunk curves toward the stimulated side. Answer 2 shows a figure for testing for a stepping response. Answer 3 shows a figure for testing for a tonic neck reflex. Answer 4 shows a figure for testing for the Moro (startle) reflex.
21. 3, 4
Rationale: Alendronate is a bisphosphonate used in hyperparathyroidism to inhibit bone loss and normalize serum calcium levels. Esophagitis is an adverse effect of primary
concern in clients taking alendronate. For this reason the client is instructed to take alendronate first thing in the morning with a full glass of water on an empty stomach, not to eat or drink anything else for at least 30 minutes after taking the medication, and to remain sitting upright for at least 30 minutes after taking it. A daily dosing schedule and a once-weekly dosing schedule is available for clients taking alendronate.
Test-Taking Strategy: Focus on the subject, the correct method to take alendronate. Recall that the primary concern with alendronate is esophagitis. Eliminate options 1 and 2 since taking with food and taking at bedtime will each place the client at increased risk of reflux. Eliminate option 5 because alendronate should be taken first thing in the morning on an empty stomach.
Review: Bisphosphonate administration
Level of Cognitive Ability: Evaluating
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Evaluation
Content Area: Pharmacology—Endocrine Medications
Priority Concepts: Client Education; Safety
Reference: Burchum, Rosenthal (2016), pp. 877–878.
22. 1, 3, 4
Rationale: Nursing interventions after a hemorrhoidectomy are aimed at management of pain and avoidance of bleeding and incision rupture. Stool softeners and a high-fiber diet will help the client to avoid straining, thereby reducing the chances of rupturing the incision. An ice pack will increase comfort and decrease bleeding. Options 2 and 5 are incorrect interventions.
Test-Taking Strategy: Focus on the subject, postoperative hemorrhoidectomy care. Recall that decreasing fluid intake will cause difficulty with defecation because of hard stool. Recognize that Fowler’s position will increase pressure in the rectal area, causing increased bleeding and increased pain.
Review: Care of the client following hemorrhoidectomy
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Adult Health—Gastrointestinal
Priority Concepts: Elimination; Pain
Reference: Ignatavicius, Workman (2016), pp. 1164–1165.
23. 1, 2, 3, 5
Rationale: Foods that decrease lower esophageal sphincter (LES) pressure and irritate the esophagus will increase reflux and exacerbate the symptoms of GERD and therefore should be avoided. Aggravating substances include coffee, chocolate, peppermint, fried or fatty foods, carbonated beverages, and alcohol. Options 4 and 6 do not promote this effect.
Test-Taking Strategy: Focus on the subject, substances that increase lower esophageal pressure. Use knowledge of the effect of various foods on LES pressure and GERD. However, if you are unsure, select the options that identify the most healthful food
item(s).
Review: The dietary regimen for a client with gastroesophageal reflux disease (GERD)
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Teaching and Learning
Content Area: Adult Health—Gastrointestinal
Priority Concepts: Client Education; Inflammation
Reference: Ignatavicius, Workman (2016), pp. 1112–1113.
24. b.
Rationale: The client has gained 5 lb in 3 days with a steady increase in blood pressure. The client is exhibiting signs of heart failure and if the client is short of breath, this will be another sign. Asking how the client is feeling is too general and a more focused question will quickly determine the client’s current health status. The scales should be calibrated periodically, but a 5 lb weight gain, along with increased blood pressure, is not likely due to problems with the scale. The weight gain is likely due to fluid retention, not drinking too much fluid.
25. 1, 2, 3, 5
Rationale: Rifabutin may be prescribed for a client with active MAC disease and tuberculosis. It inhibits mycobacterial DNA-dependent RNA polymerase and suppresses protein synthesis. Side and adverse effects include rash, gastrointestinal disturbances, neutropenia (low neutrophil count), red orange–colored body secretions, uveitis (blurred vision and eye pain), myositis, arthralgia, hepatitis, chest pain with dyspnea, and flulike syndrome. Vitamin B6 deficiency and numbness and tingling in the extremities are associated with the use of isoniazid.
Test-Taking Strategy: Focus on the subject, side and adverse effects of rifabutin. Specific knowledge is needed to answer correctly. Remember that hepatitis, flulike syndrome, neutropenia, and uveitis can occur.
Review: Rifabutin
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Pharmacology—Respiratory Medications
Priority Concepts: Clinical Judgment; Safety
References: Hodgson, Kizior (2015), p. 1052; Lilley et al. (2014), p. 678.
26. 1, 2, 3, 4
Rationale: Pulmonary edema is a life-threatening event that can result from severe heart failure. In pulmonary edema, the left ventricle fails to eject sufficient blood, and pressure increases in the lungs because of the accumulated blood. Oxygen is always prescribed, and the client is placed in a high Fowler’s position to ease the work of breathing. Furosemide, a rapid-acting diuretic, will eliminate accumulated fluid. A Foley catheter is inserted to measure output accurately. Intravenously administered morphine sulfate reduces venous return (preload), decreases anxiety, and also reduces the work of breathing. Transporting the client to the coronary care unit is not a priority intervention. In fact, this may not be necessary at all if the client’s response to treatment is successful.
Test-Taking Strategy: Note the strategic word, priority, and focus on the client’s diagnosis. Recall the pathophysiology associated with pulmonary edema and use the ABCs—airway–breathing–circulation—to help determine priority interventions.
Review: Priority interventions for the client with pulmonary edema
Level of Cognitive Ability: Synthesizing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Implementation
Content Area: Critical Care—Emergency Situations/Management
Priority Concepts: Gas Exchange; Perfusion
Reference: Ignatavicius, Workman (2016), pp. 688–689.
27. 1, 3, 5, 6
Rationale: Following eye surgery, some scratchiness and mild eye discomfort may occur in the operative eye and usually is relieved by mild analgesics. If the eye pain becomes severe, the client should notify the surgeon because this may indicate hemorrhage, infection, or increased intraocular pressure (IOP). The nurse also would instruct the client to notify the surgeon of increased purulent drainage, increased redness, or any decrease in visual acuity. The client is instructed to place an eye shield over the operative eye at bedtime to protect the eye from injury during sleep and to avoid activities that increase IOP, such as bending over.
Test-Taking Strategy: Focus on the subject, postoperative care following eye surgery. Recalling that the eye needs to be protected and that increased IOP is a concern will assist in determining the home care measures to be included in the plan.
Review: Cataract extraction with intraocular implant
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Teaching and Learning
Content Area: Adult Health—Eye
Priority Concepts: Client Education; Safety
Reference: Lewis et al. (2014), p. 395.
28. 1, 2, 4
Rationale: Hemiparesis is a weakness of one side of the body that may occur after a stroke. It involves weakness of the face and tongue, arm, and leg on one side. These clients are also aphasic: unable to discriminate words and letters. They are generally very cautious and get anxious when attempting a new task. Complete bilateral paralysis does not occur in hemiparesis. The client with right-sided hemiparesis has weakness of the right arm and leg and needs assistance with feeding, bathing, and ambulating.
Test-Taking Strategy: Focus on the subject, right-sided hemiparesis. Recalling that hemiparesis indicates weakness on one side of the body and focusing on the subject will direct you to the correct option. Also, noting the word complete in the question will assist you in answering correctly.
Review: Hemiparesis
Level of Cognitive Ability: Analyzing
Client Needs: Physiological Integrity
Integrated Process: Nursing Process—Assessment
Content Area: Adult Health—Neurological
Priority Concepts: Functional Ability; Intracranial Regulation
Reference: Ignatavicius, Workman (2016), p. 934.
29. 1, 2, 5, 6
Rationale: Seizure precautions may vary from agency to agency, but they generally have some common features. Usually, an airway, oxygen, and suctioning equipment are kept available at the bedside. The siderails of the bed are padded, and the bed is kept in the lowest position. The client has an intravenous access in place to have a readily accessible route if antiseizure medications must be administered, and as part of the routine assessment the nurse should be checking patency of the catheter. The use of padded tongue blades is highly controversial, and they should not be kept at the bedside. Forcing a tongue blade into the mouth during a seizure more likely will harm the client who bites down during seizure activity. Risks include blocking the airway from improper placement, chipping the client’s teeth, and subsequent risk of aspirating tooth fragments. If the client has an aura before the seizure, it may give the nurse enough time to place an oral airway before seizure activity begins.
Test-Taking Strategy: Focus on the subject, seizure precautions. Evaluate this question from the perspective of causing possible harm. No harm can come to the client from any of the options except for placing the bed in the high position and using a tongue blade.
Review: Seizure precautions
Level of Cognitive Ability: Analyzing
Client Needs: Safe and Effective Care Environment
Integrated Process: Nursing Process—Planning
Content Area: Adult Health—Neurological
Priority Concepts: Intracranial Regulation; Safety
Reference: Ignatavicius, Workman (2016), pp. 860–862.
30. 0.85 mL
Solution:
First convert pounds (lb) to kilograms (kg) by using the formula:
1 kg = 2.2 lb [187 lb ÷ 2.2 = 85 kg].
The physician’s order is for the client to receive enoxaparin (Lovenox) 1 mg/kg. Therefore, the client is to receive 85 mg. The desired dose in milliliters then can be calculated by using the formula of desired dose (D) divided by dose or strength of dose on hand (H) times volume (V).
85 (mg) x 0.3 mL = 25.5 mg/mL
25.5 mg ÷ 30 = 0.85 mL.
References
- Billings, D. and Hensel, D., 2019. Lippincott Q & A Review For NCLEX-RN. 13th ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Rupert, D., 2019. Lippincott NCLEX-RN Alternate-Format Questions. 3rd ed. St. Louis, MO., USA.: Wolters Kluwer Medical.
- Silvestri, L., Silvestri, A. and Turchin, L., 2020. Saunders Q & A Review For The NCLEX-RN Examination. 8th ed. Elsevier.