Placenta previa is the abnormal implantation of the placenta in the lower uterine segment, where it encroaches on the internal cervical os. One of the most common causes of bleeding during the second half of the pregnancy, this disorder occurs in about 1 in 200 pregnancies more commonly in multi gravidas than in primigravidas. If the patient has heavy maternal bleeding and then is diagnosed with placenta previa the pregnancy must be terminated.
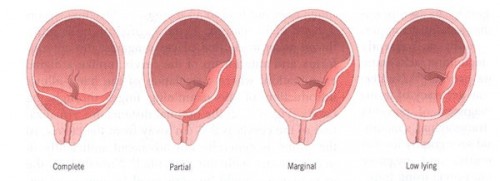
Classification of Placenta Previa
- Low Lying – The placenta implants in the lower uterine segment but does not reach the cervical os; often this type of placenta previa moves upward as the pregnancy progresses, eliminating bleeding complications later.
- Marginal– The edge of the placenta is at the edge of the internal os; the mother may be able to deliver vaginally.
- Partial– The placenta partially covers the cervical os; as the pregnancy progresses and the cervix begins to efface and dilate, bleeding occurs.
- Total– The placenta covers the entire cervical os; usually requires an emergency cesarean section.
Causes
Although the specific causes of placenta previa are unknown, factors that may affect the attachment of the placenta to the uterine wall may include the following:
- Multiparity
- Uterine scars from previous Cesarian section
- Induced or spontaneous abortions involving suction curettage
- Advanced Maternal age (>35 years)
- Cigarette smoking
- Endometritis
Sign and Symptoms
The main symptoms of placenta previa usually produce painless, bright red vaginal bleeding after 27-32 weeks of pregnancy. However uterine pain and contractions do not preclude the diagnosis in a woman who presents with vaginal bleeding. In many cases, placenta previa remains asymptomatic throughout pregnancy.
Diagnosis
Tests used to diagnose placenta previa include:
Diagnostic imaging
- Transvaginal ultrasound– a small tube placed inside the vagina to look for the uterus it usually shows how close the placenta in the edge or top of the cervix. Most beneficial for those patients with posterior placenta previas because of increased clarity of diagnosis, decreased time of scanning, and no increased incidence of hemorrhage.
- Abdominal ultrasound – a small device used to show the picture of the uterus, it’s usually done in a full bladder test.
- Doppler ultrasound– A Doppler ultrasound is usually done to check if the placenta has grown into the wall of the uterus.
- Magnetic resonance imaging– During magnetic resonance imaging (MRI), pictures are taken of the pelvis. MRI pictures may show where the placenta is in the uterus and also show how deep the placenta has grown into the uterine wall.
Lab Test
- CBC – to look for maternal anemia
- Kleihauer-Betke test – can be helpful to determine if fetal-maternal hemorrhage has occurred (detects fetal red blood cells in the maternal circulation)
- Maternal Blood Type and Antibody screen – if Rh negative will need Rh immune globulin
- APTT,PT, and Fibrin degradation products – to rule out DIC (disseminated intravascular coagulation – rare with Previa but may occur with massive hemorrhage)
Management
Management of patients with placenta previa is determined by the degree of placenta previa present, the gestational age of the fetus, and the presence and amount of vaginal bleeding.
In cases of severe hemorrhage, delivery is undertaken despite the gestational age of the fetus. Volume resuscitation and transfusion of blood products frequently are required. An emergency cesarean section delivery is performed to prevent further blood loss that could occur with disruption of the placenta previa during vaginal delivery.
Emergency Measures for Placenta Previa with hemorrhage:
- Notify M.D. immediately
- Check blood pressure, pulse and fetal heart rate immediately and every 15 minutes
- Stay with and reassure the patient
- Place patient in lateral position
- Start IV of normal saline
- Administer oxygen by tight face mask at 8-10 liters/min.
- Notify Labor and Delivery that patient is being transported to the Delivery Room