Maternity nursing is concerned with more than just a healthy and uncomplicated pregnancy. It is also worried about caring for women carrying high-risk pregnancies and ensuring that the patient can deliver safely despite these complications. Furthermore, when caring for patients with complicated pregnancies, it is important that the nurse is aware of the pregnant woman and the fetus inside her.
A high-risk pregnancy can be caused by several factors classified as physical, psychological, and social. In some cases, only one of these factors is visible, whereas, in others, a combination of two or all is present. These are the factors:
Physical Factors
- Age at the onset of gestation: below 18 years old or above 38 years old
- Being overweight or obese
- Malnutrition or being underweight
- Misshapen or inadequate pelvic structure
- Positive history of pelvic inflammatory diseases
- Cephalopelvic disproportion
- Incompetent form, position, or structure of the uterus
- Blood disorders, Rh incompatibility, and anemia
- Bleeding problems
- History of cigarette and alcohol abuse
- Hypertension, coronary artery diseases, and cardiac anomalies
- Habitual abortions and other obstetrical problems
- Trauma and previous abdominal surgeries
Psychological Factors
- Drug abuse (cocaine, methamphetamine, and other similar drugs)
- Mental illness and intake of psychotropic drugs
- Inadequate coping mechanism
- Stress and anxiety about the pregnancy
- Emotional unpreparedness for the pregnancy, labor, and delivery
- Denial of pregnancy
- Traumatic experience of previous pregnancy or loss of the fetus
- Domestic violence
Social Factors
- Low socioeconomic status
- Lack of access to proper health care services
- Poor living environment
- Isolated living areas with a lack of access to adequate transportation
- Lack of a good support system
- Exposure to chemical and physical hazards at work
- Personal or family beliefs about health
Requisites of Care for the High-Risk Pregnant Woman
Care for a high-risk pregnant patient necessitates more than a basic understanding of pregnancy, labor, and delivery. It also entails having the necessary knowledge, training, and experience in dealing with a complicated pregnancy and childbirth situation because these patients’ circumstances will provide safe and effective care.
- The right experience in monitoring fetal heart rates, contractions, and other fetal and maternal health indicators matters. Complications would be better prevented or managed if the nurse knows precisely the signs and symptoms to assess for and consider as warning signs.
- Having more than just the required competence as a maternity nurse can spell a big difference in caring for patients with high-risk pregnancies.
- Patient educator. A large number of patients in high-risk pregnancies are not equipped with the right information on how to care for themselves properly. In dealing with these patients, patient education must be provided to understand and easily relate to.
- Member of a collaborative team. Much of the care for patients does not rest solely on the nurses’ shoulders. In most cases, these care requisites include coordination and collaboration with other healthcare professionals such as physicians, medical technologists, nutritionists, pharmacists, psychologists/psychiatrists, and others.
- Caring compassionately. It can sometimes be challenging to care for a patient in a high-risk condition, especially when an unborn fetus is also to consider.
Common Conditions
There are differences in the goals of care for each condition that accompanies a high-risk pregnancy. Below are the most common diseases and other co-morbid conditions and the nursing interventions that are implemented.
Hyperemesis Gravidarum. The main problem with hyperemesis gravidarum is intractable nausea and vomiting that the patient experiences beyond the first trimester of pregnancy. These episodes result in a depletion of fluids and electrolytes, as well as a nutritional imbalance. The leading cause of this is the adverse reaction of the patient’s body to the effects of hCG.
- Signs and symptoms
- Nausea and vomiting that is more pronounced during the morning, but may persist throughout the day.
- Weight loss
- Dehydration and fluid and electrolyte imbalances
- Lack of appetite
- Tooth discoloration (in some cases; due to the effect of gastric acids in the tooth enamel)
- Interventions
- Manage nausea and vomiting
- Administer medications as may be prescribed- antiemetic (metoclopramide)
- Advise to take ice chips- decreases sensitivity in the vomiting center
- Monitor intake and output; correct fluid and electrolyte imbalances
- Ensure adequate caloric intake
- Monitor fetal well-being- FHR, activity and growth rate
- Encourage oral food and fluid intake- easily digestible carbohydrates, proteins, and other nutrient-rich food
- Advise the patient to sit up after meals to prevent the urge to regurgitate.
- Manage nausea and vomiting
Cardiac Diseases. Cardiac diseases render pregnant women problems with circulation, resulting in reduced circulatory capacity and decreased delivery of oxygen and nutrients to the tissues.
- Signs and symptoms:
- Coughing and respiratory problems (wheezing in severe cases)
- Easy fatigability and difficulty of breathing
- Palpitations
- In severe cases: edema in the lower extremities
- Chest pains or chest tightness
- Interventions:
- Check vital signs regularly, noting for heart rate and respiratory rate and effort.
- Conserve oxygen demands by limiting physical activities and alternating activities with periods of rest.
- Ensure that all signs of respiratory and cardiac symptoms are appropriately assessed and documented. Notify the physician when necessary.
- Encourage adequate food and fluid intake, increasing food rich in iron and other nutrients in the diet.
- Monitor weight gain, noting for excessive increases or decreases as this may indicate fluid retention.
- Educate the patient about monitoring for her symptoms, especially nearing the time of delivery. A caesarian section may be an option for delivery when the patient’s condition calls for it.
Gestational Diabetes Mellitus. This condition only happens during the second and third trimesters (24 to 28 weeks AOG) of pregnancy among patients who do not even have diabetes mellitus prior to pregnancy.
- Diagnosed by having the patient undergo a glucose tolerance test between the 24th and 28th week of pregnancy.
- Predisposing factors:
- Obesity
- Pregnancy at age over 35
- Family history of diabetes mellitus
- Polyhydramnios and LGA fetus
- Multiple gestations
- Signs and symptoms
- Fetus that is large for gestational age
- Glucosuria and ketonuria
- Excessive hunger and thirst
- Weight loss
- Recurrent urinary tract infections
- Blurring of vision
- Interventions in the Prenatal Period
- Ensure adequate weight gain through correction of diet and encouraging light to moderate physical activity.
- Maintain blood glucose levels between 65mg/dL to 130mg/dL (3.7 to 130mmoL).
- Monitor signs of increased blood sugar levels: ketonuria, glucosuria, hyperglycemia.
- If with insulin therapy: ensure administration with the time and dosage prescribed.
- Protect the patient from infection and resolve any infection present.
- Monitor fetal well-being regularly: FHR, amniotic fluid index, movements.
- Interventions during Labor
- Ensure that the patient is hooked to the fetal monitor to assess fetal well-being during labor.
- Prepare and position the patient for delivery (either vaginal or Caesarian section) and ensure that insulin administration is properly calibrated throughout delivery.
- Interventions during the Postpartum Period
- Monitor the patient closely for indications of a hypoglycemic reaction.
- Correct blood glucose problems through insulin administration, IV fluids and diet.
- Evaluate patient response to delivery and therapy and report any complications to the physician.
Human Immunodeficiency Virus (HIV) and Acquired Immune Deficiency Syndrome (AIDS). HIV is a virus that is responsible for causing AIDS. It is sexually transmitted and may be passed on from the mother to her fetus. In some cases, when the HIV infection has progressed into full-blown AIDS, the patient presents with several complications that may threaten the pregnancy.
- Most individuals with HIV infections acquire it from unsafe sexual practice, sharing of infected needed (especially among drug users), through blood transfusion or placental transmission.
- Zidovudine is the drug of choice, especially among pregnant women, to help prevent maternal-to-fetal transmission of the disease. This is usually given in the second trimester (14th-week AOG) via an oral route and through IV during labor and delivery. The neonate born of an HIV-positive mother receives the drug 6 weeks after birth through oral drops (syrup).
- Because of the nature of HIV infections, the patient is also monitored to detect and prevent opportunistic infections.
- Signs and Symptoms vary according to the stage of infection the patient is in.
- Diagnosis of HIV/AIDS:
- ELISA- a screening test for the presence of viruses in the blood sample of the patient. A positive result for ELISA does not necessarily mean a positive test for HIV/AIDS
- Western Blot- confirmatory test for HIV/AIDS
- Interventions for the mother with HIV/AIDS:
- Monitor closely for vital signs, noting for any indication of infection and other complications from HIV
- Prevent opportunistic infections from occurring- isolate the patient when necessary
- Encourage adequate nutrient and fluid intake.
- Monitor weight closely, avoid excessive weight gain.
- Provide psychosocial support- stress, anxiety and depression are common mental health issues for the patient.
- Prepare for Caesarian delivery- vaginal delivery increases the likelihood of the fetus contracting the infection through the birth canal.
- Protect the patient from bleeding and infections during delivery
- Administer medications diligently (Zidovudine, anti-infectives, etc.)
- Instruct the patient care requisites for her newborn during the third trimester:
- Zidovudine syrup from 6 weeks onwards
- HIV culture to be taken at the first and fourth months of life to determine if the child is positive for the disease and determine viral counts
- Monitoring the infant for signs and symptoms of HIV and reporting them to the physician
Disseminated Intravascular Coagulation (DIC). A hemorrhagic disorder of pregnancy, DIC, is caused by systemic coagulation activation in response to a bleeding problem. The condition then cascades into the formation of clots in the microcirculation, depleting the body of platelets and clotting factors. This leads to internal hemorrhage and, if not appropriately resolved, could cause the patient’s death.
- Predisposing factors:
- Hemorrhagic disorders of pregnancy
- Abruptio placentae
- Placenta previa
- Gestational hypertension
- Intrauterine fetal death
- HELLP syndrome
- Amniotic fluid embolism
- Liver disorders and Sepsis
- Signs and symptoms
- Ecchymosis, purpura or bruising even in the absence of trauma
- Unabated bleeding
- Traces of bleeding in stool or vomitus
- Excessive vaginal bleeding
- Decreasing platelet counts and hematocrit levels
- Increased prothrombin, partial thromboplastin and clotting times
- Interventions
- Ascertain the underlying cause of bleeding and correct it.
- Monitor vital signs closely, assessing carefully for signs of excessive bleeding and impending shock.
- Administer oxygen therapy as prescribed
- Prepare for the administration of blood transfusion, heparin therapy and IV fluids (to replace circulating fluid volume)
- Hemorrhagic disorders of pregnancy
Ectopic Pregnancy. An ectopic pregnancy occurs when the fertilized ovum is implanted outside the uterine cavity. The most common site for ectopic pregnancy is in the ampulla of the fallopian tube.
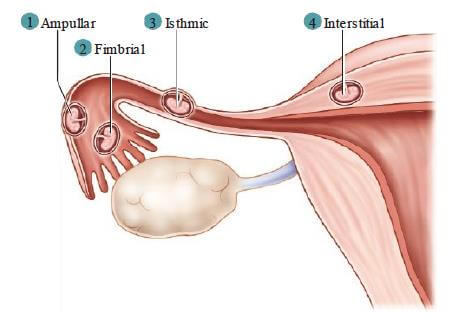
- Risk factors
- Maternal age over 35 years old
- Previous abdominal or pelvic surgery
- History of multiple abortions
- Endometriosis
- History of pelvic inflammatory diseases
- Certain sexually transmitted infections
- Signs and symptoms
- Dull or aching abdominal pain
- Missed menstrual periods
- Positive pregnancy test (hCG)
- Dark red to brownish vaginal bleeding or spotting
- NOTE: when the ectopic pregnancy ruptures, the patient reports sudden, knifelike pain, referred pain along the shoulder, and exhibits signs of shock (hypotension, tachycardia, tachypnea; decreasing levels of consciousness).
- Interventions
- Monitor vital signs closely and assess for the presence of lower abdominal pain
- Anticipate an order for methotrexate administration (The drug is administered to inhibit cellular division in the developing embryo, leading to embryonic death).
- Anticipate an order to prepare the patient for surgical termination of the ectopic pregnancy: laparotomy with removal or repair of the affected fallopian tube
- Administer antibiotics and other medications as may be prescribed.
- Provide the patient and family psychosocial support
- Refer the patient to a counselor if needed
Hydatidiform Mole (H-mole). An H-mole is a gestational trophoblastic disease that is usually detected in the second trimester of pregnancy. The main presentation is the presence of grape-like clusters of tissues that are clumped together. These are filled with fluid inside and may or may not be malignant.
- Signs and symptoms
- Signs indicative of pregnancy- (+) hCG test, increase in fundal height (typically more significant than expected AOG), missing periods.
- Absent fetal heart rate on doppler
- Ultrasound reveals the presence of grape-like clusters instead of a fetal outline.
- Vaginal bleeding, usually more pronounced towards the fourth week or until the second trimester
- Increased blood pressure, (+) proteins in the urine- indicates pre-eclampsia.
- Interventions
- Monitor vital signs, especially blood pressure
- Anticipate an order for the evacuation of the H-mole
- Vacuum aspiration
- Administer oxytocin after aspiration to keep the uterus contracted- prevents hemorrhage.
- Send tissue samples of the mole for histologic testing and determining malignancy.
- Monitor hCG levels every 2 weeks until normal levels are reached. Check levels once a year until the first year after evacuation.
- Teach patient and partner about birth control measures. NOTE: The patient is advised to prevent pregnancy during the 1-year monitoring period.
Abortion. An abortion is defined as a pregnancy terminated prior to 20 weeks of gestation, or when a fetus reaches the age of viability. This can happen spontaneously or may be done electively.
- Types of abortion
- Spontaneous. The termination of pregnancy due to natural causes.
- Induced. An abortion occurs as part of a therapeutic or elective procedure. It is usually a result of administering a mix of medications to trigger uterine contractions.
- Threatened. Characterized by the presence of cramping sensation and light vaginal bleeding but without any change to the cervix.
- Inevitable. It is marked by the presence of cramping and vaginal bleeding with accompanying cervical effacement and opening.
- Incomplete. An abortion in which several fragments of the fetus or the placenta are still retained in the uterus. This necessitates an evacuation.
- Complete. The fetus and all other products of conception are removed from the uterus.
- Missed. Abortion that has happened without apparent symptoms. This requires induction and removal of all the products of conception.
- Habitual. Occurs when abortion occurs in 3 or more successive pregnancies. It may indicate another problem: uterine structure, hormonal imbalances, autoimmune disorders, etc.
- Signs and symptoms
- Spontaneous vaginal bleeding
- Presence of mild to moderate lower abdominal pain
- Uterine contractions (intensity may vary)
- Passage of blood or clots through the vagina
- In some cases, the fetus may also be expelled from the vaginal opening.
- Interventions
- Assess and document vital signs, including pain
- Check for blood clots in the perineal pads; count the number of pads the patient used. Save any expelled tissues and clots if needed.
- Maintain patient on bed rest
- Keep IV line patent and administer fluids and medications as prescribed.
- If products of conception are still retained in the uterus, prepare the patient for dilation and curettage.
- Provide psychological support to the patient and significant others
TORCH Syndrome. A combination of multiple infections that threaten the well-being of both mother and fetus. These infections include:
- An infection brought about by the protozoa Toxoplasma gondii, resulting in an acute flu-like infection to the mother. The agent is usually contracted through ingestion of raw meat or handling cat litter. The infection may cause spontaneous abortion in the first trimester or can be passed from the mother to the fetus through the placenta.
- Other infections. May include HIV, AIDS, Hepatitis B, and other sexually transmitted diseases; West Nile virus, and others.
- Also known as German Measles, this infection is considered teratogenic, especially in the first trimester, affecting the fetus’s eyes, heart, ears, and brain. May cross the placental barrier.
- Transmitted through close contact, CMV infections may also be transferred from the mother to the fetus via the placenta or during delivery through contact with the birth canal. Infection may cause low birth weights among infants, enlargement of the spleen and liver, jaundice, hearing loss, blindness, and seizure disorders.
- Herpes simplex virus. This infection typically causes the formation of painful fluid-filled vesicles and the external genitalia and may be transmitted from the mother to the infant during vaginal delivery. If a patient is diagnosed with this infection, delivery is usually done via a caesarian section and vaginal exams are discouraged. Contact precautions are also observed.
Multiple Gestation. Also known as multiple pregnancies, this occurs when fertilization occurs for 2 ova (fraternal or dizygotic) or when a single fertilized ovum splits into two or more (identical or monozygotic). Multiple gestations place increased physical stress for the mother as she needs her body to cope with the growth and development of two or more fetuses.
- Signs and symptoms
- Presence of excessive fetal activity
- A uterus that is larger for gestational age
- Multiple fetal outlines in ultrasound
- Several large parts of the fetus felt upon palpation
- Multiple fetal heart rates were recorded upon auscultation
- Excessive weight gain for the mother
- Interventions
- Monitor maternal well-being: vital signs, weight gain, fluid and nutrient intake; monitor for symptoms of anemia
- Monitor fetal well-being: fetal heart rates, fetal activity, and growth patterns, amniotic fluid index
- Prepare the patient for ultrasound, as recommended
- Increase intake of vitamin supplements and iron preparations as needed
- Assess for symptoms suggesting preterm labor, abortion, and other complications
- Prepare for possible caesarian delivery
- Provide emotional support to the patient and significant others.
Conclusion
It is a challenge to care for a pregnant woman and more challenging to care for a patient who has a high-risk pregnancy. However, armed with the proper knowledge and a sincere desire to provide safe, quality, and effective care, the nurse, can help these patients successfully bring their pregnancies to term and deliver a healthy infant into the world.
References
- Perry, S. E., Hockenberry, M. J., Lowdermilk, D. L., & Wilson, D. (2014). Maternal child nursing care.
- Perry, S., & Olshansky, E. (2018). Maternal Child Nursing Care (6th ed.). Mosby. Elsevier.
- Ricci, S. S., Kyle, T., & Carman, S. (2013). Maternity and pediatric nursing. 2nd ed. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins.