Pneumonia is one of the most common diseases among people of all ages, especially children and older adults. Nurses play a vital role in caring for patients with pneumonia and helping to reduce these cases in the community. Nurses need to have a thorough knowledge of pneumonia, its disease process, and its management to provide effective and quality care. This article provides a comprehensive approach, including pathophysiology, for nurses and student nurses.
Pneumonia is an infection of the parenchyma of one or both lungs caused by various microorganisms, including bacteria, viruses, fungi, and chemical irritants. It is characterized by inflammation and fluid accumulation in the air sacs, leading to symptoms such as cough, chest pain, fever, and difficulty breathing.
According to the WHO, pneumonia resulted in 808,000 deaths of children under the age of 5 in 2017, accounting for 15% of all deaths in this age group. In 2019, pneumonia led to the deaths of 740,180 children under the age of 5, accounting for 14% of all deaths in this age group.
Causative Agents
Several microorganisms can cause pneumonia:
- Bacteria: The most common bacterial cause is Streptococcus pneumoniae (pneumococcal pneumonia), which can affect people of all ages, especially those with weakened immune systems.
- Viruses: Viral pneumonia can be caused by various viruses, including the flu (influenza) and respiratory syncytial virus (RSV), and is responsible for about one-third of all pneumonia cases.
- Fungi: Fungal pneumonia can result from conditions such as valley fever, caused by the Coccidioides fungus.
- Other causes: Aspiration pneumonia occurs when food, liquids, or stomach contents are inhaled into the lungs.
Type of Pneumonia
There are different types of pneumonia depending on the setting or environment where it is acquired:
- Community-Acquired Pneumonia (CAP): This type of pneumonia develops in the community setting within the first 48 hours. Common causes include bacteria like Streptococcus pneumoniae, Haemophilus influenzae, and atypical pathogens like Mycoplasma pneumoniae and Chlamydia pneumoniae.
- Hospital-Acquired Pneumonia (HAP): This type of pneumonia develops 48 hours or more after hospital admission following an illness or a procedure and is often caused by more antibiotic-resistant pathogens like Staphylococcus aureus, Pseudomonas aeruginosa, and Klebsiella pneumoniae. This type of pneumonia can be fatal and hard to treat.
- Ventilator-Associated Pneumonia (VAP): This type of pneumonia is acquired more than 48 hours after endotracheal intubation and mechanical ventilation. The pathogens are similar to those causing HAP but also include Acinetobacter species.
- Healthcare-Associated Pneumonia (HCAP): HCAP is acquired when residing in an extended-stay outpatient clinic or a long-term care facility (such as a nursing home). Similar to pneumonia obtained in a hospital, antibiotic-resistant bacteria are typically the main cause.
- Aspiration Pneumonia: This type of pneumonia is caused by the ingestion of gastric contents, solid food, or liquid that enters the throat and goes directly to the lungs. This condition is often seen in patients with impaired gag reflexes and people with swallowing difficulties.
Risks
Although pneumonia can affect anyone, certain groups are at higher risk of acquiring pneumonia:
- Young children: Children under 5 years of age are more susceptible to acquiring pneumonia and other infections because their immune systems are still developing.
- Older adults: Adults aged 60 years and above are also more prone to acquiring pneumonia due to declining immune systems, especially those with other comorbidities.
- People with underlying health conditions: People with conditions such as cystic fibrosis, chronic obstructive pulmonary disease (COPD), asthma, and conditions affecting the kidneys, heart, or liver are more susceptible to acquiring infections such as pneumonia due to damage to the lungs and difficulty clearing out germs.
- People diagnosed with impaired immune systems: People diagnosed with HIV/AIDS, cancer, or taking immunosuppressive medications have weak immune systems, thus lowering the body’s ability to fight infection. Cancer treatments like chemotherapy and immunosuppressive medications used for conditions like autoimmune diseases can weaken the immune system.
- Smokers and heavy drinkers: Smoking and heavy alcohol drinking can weaken the lungs and increase the risk of infection.
Diagnostic Procedure
A pneumonia diagnosis can be tricky. While there isn’t a single definitive test for it, doctors can use a combination of methods to diagnose pneumonia. Here are some diagnostic tests commonly used to confirm the presence of pneumonia:
- Chest X-ray: This is a quick and painless imaging test that healthcare professionals utilize to determine if there’s fluid or pus in the lungs, which is a sign of pneumonia.
- Physical exam: During a physical exam, the doctor will listen to the lungs of the patient using a stethoscope. Pneumonia can cause crackling sounds in the lungs. They’ll also check vital signs such as temperature, heart rate, and breathing rate. An abnormal breathing rate (tachypnea) is a common sign of pneumonia.
- Sputum test: If the patient is coughing up mucus (phlegm), the doctor might ask to collect a sample of it. They’ll then send it to a lab to see if it contains bacteria or viruses that cause pneumonia.
- Blood tests: While blood tests can’t diagnose pneumonia on their own, these tests can help the doctor determine if there is an infection and what kind of infection it is.
- Pleural fluid test: In some cases, the doctor might need to do a pleural fluid test. This involves inserting a needle into the space between the two layers of tissue that line the lungs (pleural space) to collect a fluid sample. The fluid will then be sent to a lab for testing.
As a nurse, if you see a patient experiencing any potential pneumonia symptoms, it is best to instruct them to see the doctor right away to get a proper diagnosis and treatment plan. Early diagnosis and treatment can help prevent the development of complications.
Treatment
Treatment for pneumonia depends on the type of infection. If the cause of the infection is bacterial, antibiotics are used to treat bacterial pneumonia, which helps speed recovery from mycoplasma pneumonia in some cases. While most viral pneumonias do not have a specific treatment and resolve on their own, antivirals may be used in some cases. Antifungal medications are used to treat fungal pneumonia, which may require a longer period of treatment.
Complications
Pneumonia can lead to various complications if not treated early, especially in those with weakened immune systems or chronic conditions. Below are some of the complications that result from untreated or chronic pneumonia:
- Empyema: Infection of the space between the membranes surrounding the lungs and chest cavity.
- Pericarditis: Inflammation of the sac surrounding the heart.
- Endobronchial obstruction: Blockage of the airway that allows air into the lungs.
- Atelectasis: Collapse of an entire lung or an area within the lung.
- Lung abscess: Collection of pus in the lungs.
- Pleurisy: Inflammation of the thin membranes between the lungs and ribcage.
- Septicemia: Infection in the blood that originated elsewhere in the body.
- Sepsis: A life-threatening immune reaction to septicemia.
- Worsened chronic conditions: Pneumonia can exacerbate conditions like congestive heart failure and emphysema.
- Death: In severe cases, pneumonia can be fatal, especially in vulnerable populations like young children and older adults.
Prevention
All will agree that prevention is better than cure. The following activities are part of preventive measures against pneumonia:
- Vaccination
Vaccines to prevent pneumococcal disease are available in the community setting and in government or private hospitals and clinics. There are many kinds of vaccines depending on the strain causing pneumonia. - Good hygiene
Practicing good hygiene, such as washing hands regularly, can help prevent the spread of infection. - Avoiding smoking and heavy drinking
Quitting smoking and reducing alcohol consumption can help reduce the risk of developing pneumonia because putting a stop to these habits aids in strengthening the immune system. - Maintaining a healthy diet and lifestyle
Eating a balanced diet and staying physically active can help boost the immune system, thus lowering the chance of being infected with pneumonia.
Nursing Care for Patients with Pneumonia
These nursing interventions help manage symptoms, prevent complications, and support the patient’s recovery from pneumonia.
Promoting Respiratory Health
- The nurse should encourage patients to drink plenty of fluids, at least 2-3 liters per day, to help loosen pulmonary secretions and stay hydrated.
- Use humidifiers to add moisture to the air, which can help break up mucus and make breathing easier.
- Teach patients effective coughing techniques to clear their airways and improve airway patency.
- Perform chest physiotherapy to help mobilize and remove secretions, making it easier for patients to breathe.
- The nurse should position patients in a semi-Fowler’s position, which allows for easier breathing and lung expansion, and change positions frequently to enhance secretion clearance and improve pulmonary ventilation and perfusion.
Supporting Rest and Recovery
- Advise patients to avoid overexertion and possible exacerbation of symptoms, encouraging them to rest as much as possible.
- Monitor oxygen levels regularly using pulse oximetry and administer oxygen as prescribed to ensure adequate oxygenation.
- It is important to avoid administering cough suppressants, as they can prevent the body from clearing secretions and lead to reinfection.
Ensuring Proper Nutrition
- Ensure that the patient is provided with fluids with electrolytes to help restore proper nutrition and support the immune system.
- Offer nutritionally enhanced drinks and shakes to boost caloric and nutrient intake, which is crucial for recovery.
Education and Support
- One of the roles of nurses in taking care of patients diagnosed with pneumonia is to educate patients and their families about the cause of pneumonia, management of symptoms, signs and symptoms to watch for, and the importance of follow-up care.
- Encourage patients to get vaccinated against pneumococcus and influenza to prevent future infections.
- Promote healthy habits like eating a balanced diet, staying active within their limits, and practicing good hand hygiene to reduce the risk of reinfection.
As nurses, we have the privilege of providing compassionate care to patients with pneumonia. We can make a significant difference in their lives by addressing their physical needs, promoting rest and recovery, ensuring proper nutrition, and offering health education and support. Remember, every small act of kindness and piece of information we share can profoundly impact our patients’ well-being and recovery.
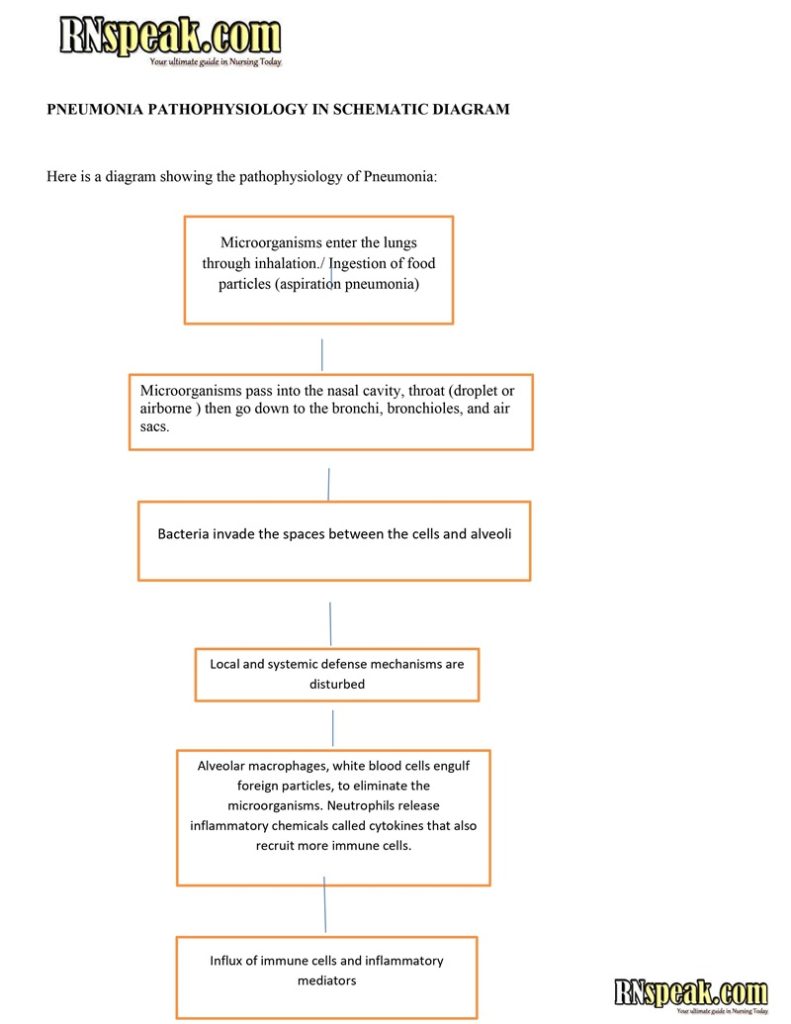
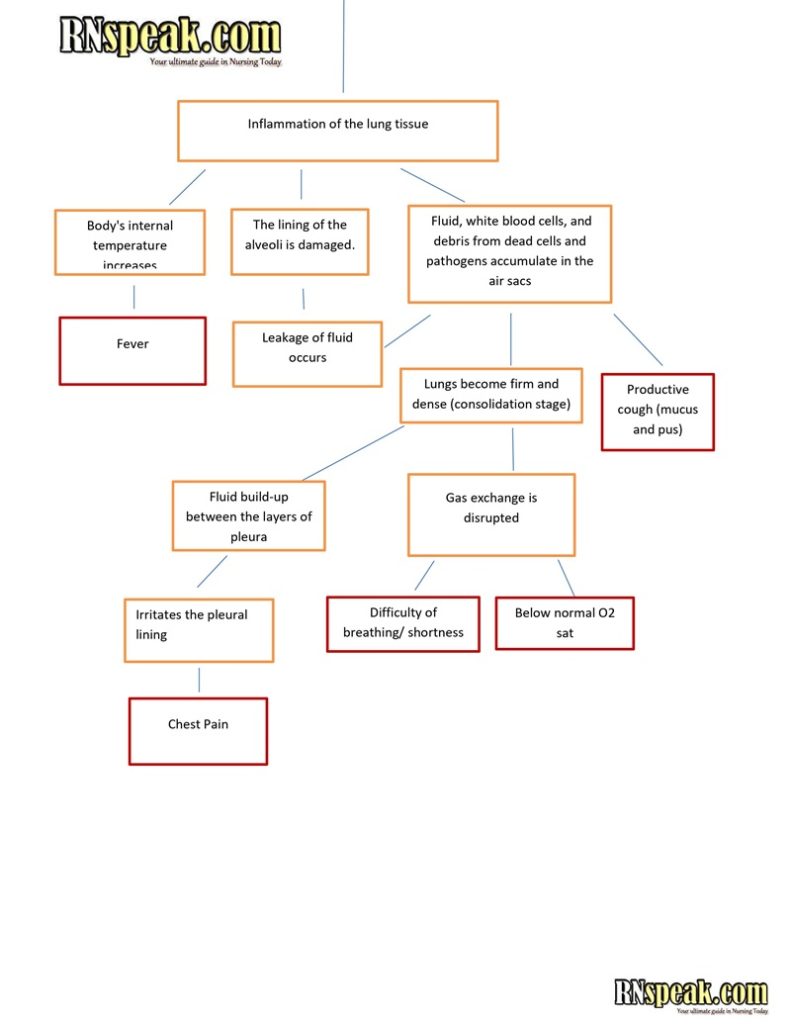
Pneumonia Pathophysiology in Schematic Diagram
References
- Hinkle, J. L., & Cheever, K. H. (2014). Brunner & Suddarth’s textbook of medical-surgical nursing (Edition 13.). Wolters Kluwer Health/Lippincott Williams & Wilkins.
- Almirall J, Serra-Prat M, Bolibar I, Balasso V. Risk Factors for Community-Acquired Pneumonia in Adults: A Systematic Review of Observational Studies. Respiration 2017; 94(3): 299-311. [PubMed]
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Overview: Pneumonia. [Updated 2021 May 18]. Retrieved from: https://www.ncbi.nlm.nih.gov/books/NBK525774/
- Pneumonia in children. (n.d.). Retrieved June 13, 2024, from Who.int website: https://www.who.int/news-room/fact-sheets/detail/pneumonia








This is a very detailed, well explained article.
Thank you for sharing your brilliant knowledge, writer.