Anaphylaxis is an alarming emergency situation because of its rapid onset which may lead to death within a short period of time. Despite its fatalities, death and the irreversible damage it caused, anaphylaxis is not always recognized thus, studies may underestimate the incidence (Soar et al, 2008). Anaphylaxis is not a reportable disease and the true incidence is unknown as concluded by Sheikh and colleagues (2012)—due to the perplexity of its diagnosis, treatment and investigation; limited data on fatal anaphylaxis; and non-compliance for outpatient follow-up of its victims. Time trends for anaphylaxis fatalities are not properly presented.
Definition
Anaphylactic shock is a severe, life-threatening, generalized or systemic hypersensitivity reaction characterized by rapidly developing critical tribulations on airway/breathing and circulation usually associated with skin and mucosal changes, as defined by the European Academy of Allergology and Clinical Immunology Nomeclature Committee. It is a circulatory shock state resulting from severe allergic reaction producing an overwhelming systemic vasodilatation and hypovolemia (Smeltzer & Bare, 2004).
Epidemiology
In the study of Soar and colleagues (2008), the American College of Allergy, Asthma and Immunology reported that the overall frequency of episodes of anaphylaxis lies between 30 and 950 cases per 100, 000 persons per year and a lifetime prevalence of between 50 and 2000 episodes per 100, 000 persons or 0.05-2.0%.
Death immediately occurs after the contact with the trigger if anaphylaxis is fatal, called anaphylactic shock. From a case-series, fatal food reactions cause respiratory arrest typically after 30-35 min; insect stings cause collapse from shock after 10-15 min; and deaths caused by intravenous medication occur most commonly within 5 min. Death never occurred more than 6 hours after contact with the trigger (Soar et al, 2008).
Causative Agents
Trigger factors include foods, insect venoms (sting), medications, anesthetics, natural rubber latex and exercise (Sheikh et al, 2012); allergens such as plant pollens, dust, mold spores and chemicals in cosmetics (Scanlon & Sanders, 2007); blood products and contrast agents (Smeltzer & Bare, 2004).
Anatomy and Physiology
Anaphylactic shock is a multisystem failure resulted from inadequate tissue perfusion involving function shut-down of cardiovascular system, respiratory system, urinary system, circulatory system, nervous system, integumentary system and gastrointestinal system. The principal reason for anaphylactic shock is the over-activity of the immune system resulting in a systemic inability to thrive.
An allergy is a hypersensitivity to a particular foreign antigen, called an allergen. When the immune system over-reacts to the allergen, it causes hypersensitivity producing tissue damage. The antigen is a chemical marker that identifies cells whether “self” or “non-self” (foreign body). Antibodies, also called immune globulins (IgE) or gamma globulins, attached to antigens to “label” them for the destruction of foreign bodies (Scanlon & Sanders, 2007).
During an allergic response, the immune system produce are IgE antibodies, which bind to mast cells. Mast cells release chemicals such as histamine and leukotrienes. These chemicals contribute to the process of inflammation by increasing the permeability of capillaries and venules. Tissue fluid collects and more WBCs are brought to the damaged area. In the case of anaphylactic shock, allergy mediators flooded the body causing severe inflammation (Scanlon & Sanders, 2007; Sheir et al, 2006).
Pathophysiology
Anaphylactic agents may enter the body through ingestion, inhalation, direct skin contact/topical, sting, transfusion and injections. Antigen will identify the allergens as non-self (foreign body). Mast cells will release chemicals and binds with antibodies IgE leading to an inflammatory reaction. Anaphylactic shock occurs when over-responding of allergy mediators occurs, causing systemic vasodilatation and increase capillary permeability resulting to poor tissue perfusion. Poor tissue perfusion and hypovolemia resulted to shock (Scanlon & Sanders, 2007; Sheir et al, 2006; Smeltzer & Bare, 2004).
Clinical Manifestations
(Sheikh et al, 2012; Soar et al, 2008; Decker et al, 2008; NHTA, 1990).
Integumentary System
– erythema – patch, generalized, red rash
-edema (localized, anasarca)
– urticaria – (hives, nettle rash, weals, welts) pale, pink or red, may look like nettle stings, different shapes and sizes, surrounded by a red flare, pruritic
– angioedema – swelling of deeper tissues in the eyelids, lips, mouth and throat
*Skin and mucosal changes often the first feature and present in over 80% of anaphylactic reactions (Soar et al, 2008).
Respiratory System
– pharyngeal/laryngeal edema
– difficulty of breathing (dyspnea) / shortness of breath
– tachypnea
– hypoventilation
– labored breathing using accessory muscles
– abnormal retractions
– prolonged expirations
– difficulty of swallowing, tightness in the throat, congestion
– hoarseness of voice
– aphonia
– stridor (upper airway)
– wheeze (lower airway)
– diminished lung sounds
– increase respiratory rate
– respiratory arrest (late stage)
Cardiovascular system
– myocardial ischemia with ECG changes
– chest pain
– presyncope, syncope
– orthostasis
– tachycardia (compensatory)
– arrhythmia (late sign)
– hypotension (late sign)
– bradycardia (late sign)
– cardiac arrest (late stage)
Nervous System
– confusion, agitation, dis-oriented, loss of consciousness
– dizziness, fainting
– seizures
Circulatory System
– cold, pale and clammy
– cyanosis (late sign)
Gastrointestinal System
– oral mucosal pruritus
– intraoral angioedema of buccal mucosa, tongue, palate or oropharynx
– nausea
– emesis
– dysphagia
– abdominal cramps
– diarrhea
Urinary System
– increase GFR
– increase urinary output (hypovolemia – late stage)
Assessment
*Not all signs and symptoms are present in every case
A. History
- previous exposure
- previous experience to exposure
- onset of symptoms
B. Presenting signs and symptoms
C. Glasgow coma scale (level of consciousness), general condition, vital signs
D. Assessment tools
- cardiac monitor
- pulse oximetry (usually low)
- end tidal CO2 (usually high)
- non-invasive blood pressure to monitor hypotension
- 12-lead ECG to monitor cardiac arrest
Diagnostic Examination
The diagnosis of anaphylaxis is based largely on history and physical findings. Laboratory procedures have proven to be not always reliable in the diagnosis. Elevated plasma histamine is only reliable within one hour of onset. Serum or plasma tryptase levels greater than 15ng/ml within 12 hours (ideally within 3 hours) of onset is more widely used as a confirmatory test but usually negative in food-induced anaphylaxis. Serial total serum or plasma tryptase measurements are more advisable that single measurement. Proven skin tests to allergens and elevated allergen-specific IgE levels in serum are not a reliable diagnostic of anaphylaxis, moreover, these tests provide clinical relevance in the prevention of anaphylaxis (Sheikh et al, 2012). Mast cell tryptase is the laboratory procedure that will confirm a diagnosis of anaphylactic reaction. Medical emergency investigations such as arterial blood gases, ECG, chest x-ray, urea and electrolytes may also be helpful in the treatment (Soar et al, 2008).
Medical Management
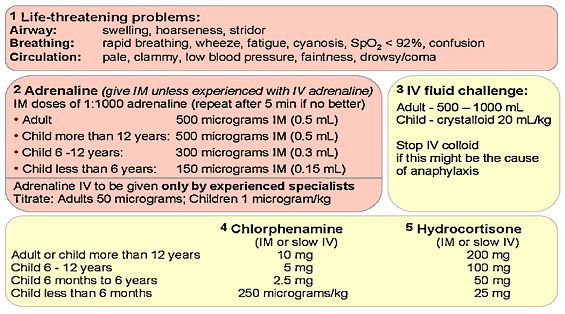
Patients having an anaphylactic reaction should be treated using the Airway, Breathing, Circulation, Disability, Exposure (ABCDE) approach (Soar et al, 2008).
Remove the trigger, if possible.
Immediate intervention for anaphylaxis is the removal of the causative agent, although it is not always feasible. Once the first sign of reaction occurs, immediately stop/discontinue any drug, infusion, and/or transfusion suspected of causing the allergic reaction. Remove the stinger after a bee sting. For food-induced anaphylaxis, force vomiting is not recommended because of the possibility of aspiration due to esophageal edema. Do not delay definitive treatment if removing the trigger is not possible (Soar et al, 2008; NHTA, 1990).
Positioning
Patients should be placed in a comfortable position to promote ventilation and circulation. Patients with airway and breathing problems may assume fowler’s position for maximal breathing (for early-stage), unless not contraindicated, e.g. hypovolemia and hypotension (late-stage). Lying flat with or without leg elevation or Trendelenburg position is helpful for patients with hypotension and other circulatory problems. Patients with anaphylactic shock should not be placed on sitting and never on standing up, as these can deteriorate the patient’s condition leading to cardiac arrest. Victims that are breathing and unconscious should be place on their side, recovery position. Pregnant patients should lie on their left side to prevent caval compression (Soar et al, 2008; NHTA, 1990). In the study of Zhao et al (2007), it was concluded that the head-down tilt posture (Trendelenburg position) can facilitate venous return from the splanchnic organs and lower extremities and is recommended for the treatment of hypotension in anaphylactic shock.
Assist on Ventilation and Advanced Airway
Due to laryngeal edema and inflammation of the bronchial passages, endotracheal intubation or tracheostomy may be necessary to establish an airway and promote ventilation (Smeltzer & Bare, 2004).
Circulation
Initiating venous access is a must for fluid resuscitation and administration of medications. The Central venous line is also important in monitoring central venous pressure.
Managing Cardio-pulmonary arrest
If the cardiopulmonary arrest occurred, CPR is immediately performed. Start CPR according to current guidelines (Soar et al, 2008; Smeltzer & Bare, 2004).
Pharmacological Management
Pharmacological treatment aims to decrease vascular permeability, restore vascular tone and provide emergency support to basic life functions (Smeltzer & Bare, 2004; NHTA, 1990).
Oxygen
Highest concentration of oxygen is immediately administered, preferably using a mask with an oxygen reservoir which gives 60%-100% O2 concentration. Use self-inflating bag for patients with tracheostomy or endotracheal tube (Soar et al, 2008). Anaphylactic shock and the other types of shock are characterized by generalized cellular hypoxia resulted from poor tissue perfusion and decrease oxygen. The severity, irreversible damage and mortality aftershock are strongly associated with depleted oxygen levels in the brain (Cui et al, 2006).
Fluid Resuscitation
Large volumes of fluid may leak from the patient’s circulation during anaphylactic reaction because of fluid shift during systemic inflammatory process and increase urinary output resulting to hypovolemia. There will also be vasodilatation. A large volume of fluid may be needed to treat hypovolemia and promote circulation. Fluid resuscitation should be infused immediately. Hartmann’s solution or 0.9% saline are advised for fluid management. Be careful with the use of colloids and crystalloids as this may cause anaphylaxis (Soar et al, 2008).
Adrenaline (Epinephrine)
Adrenaline is widely used as the first-line and main stay treatment of choice for anaphylaxis. It is administered for the purpose of its vasoconstrictive action (Sheikh et al, 2012; Soar et al, 2008; Smeltzer & Bare, 2004; NHTA, 1990).
Antihistamine
Antihistamines are the second line of treatment. Anti-histamines may help counter histamine-mediated bronchoconstriction and vasodilatation, thereby reducing capillary permeability. Chlorpheniramine maleate and Diphenhydramine are the drugs of choice for anaphylactic reaction (Soar et al, 2008; Smeltzer & Bare, 2004).
Bronchodilator
Bronchodilators can be given to reverse histamine-induced bronchospasm. Aminophylline per IV can be given for severe cases. Nebulization is administered using albuterol, salbutamol and ipratropium. Although intravenous magnesium is a vasodilator, contraindicated in anaphylactic shock since it can cause hot flushes and make hypotension worse (Soar et al, 2008; Smeltzer & Bare, 2004).
Anti-inflammatory / Immunosuppressant
Steroids management using corticosteroids may help prevent or shorten anaphylactic reactions. This works by decreasing inflammation and reducing the activity of the immune system (Soar et al, 2008; Smeltzer & Bare, 2004; NHTA, 1990).
Vasopressor
Vasopressors and inotropes (noradrenaline, vasopressin, metarminol and glucagon) are used when initial resuscitation with adrenaline and fluids are not effective. Glucagon is given for patients who are taking beta-blockers. For patients who develop severe bradycardia after an anaphylactic reaction, atropine IV can treat this condition (Soar et al, 2008)
Anaphylaxis Algorithm
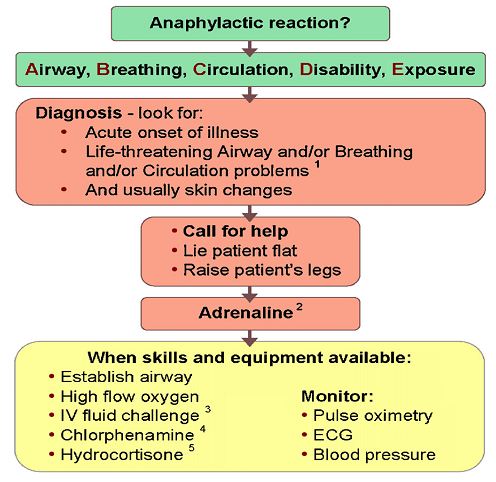
Nursing Management
Promotive and Preventive
- The nurse should identify the patient’s history on allergy, assessing patients for allergies or previous reactions to antigens plays an important role in the prevention of anaphylactic shock.
- Patient’s and family’s education to prevent further exposure to antigens and the immediate actions to be taken.
- Provide record keeping. When allergies are identified, it is important that the patient keeps a record with him/her or wear an identification band.
Curative
- Early recognition with accurate assessment and diagnosis.
- Render immediate treatment without any delay using the ABCDE approach.
- Knowledge and skills in the medical treatment and pharmacological management of anaphylactic shock.
- Expertise on IV therapy, BLS and ACLS.
Rehabilitative
- Psychological support and support system.
- Disability rehabilitation.
Complications
The most distressing complication of anaphylactic shock is the disability and the irreversible damage following poor brain tissue perfusion. Respiratory complications may occur, and patient may have tracheostomy or much worst with the support of a mechanical ventilator. Physical disability is possible, and physical rehabilitation is a must. Autoimmune disorders following prolonged medications and renal complications may occur after severe hypovolemia and anaphylactic shock.
Discharge Plan and Patient’s Education
Medications
- Compliance with medical regimen.
- Pharmacokinetics and pharmacodynamics of medications, including emphasis on actions and side-effects.
- Provide instructions and training for the patient and family on the use of adrenaline auto-injector, administration of emergency medications and injection of anti-histamine for patients with a repeated history of anaphylactic shocks and high-risk cases (Soar et al, 2008; Smeltzer & Bare, 2004)
Environment
- To prevent anaphylactic shock, avoid the triggers (allergens). Provide an allergen-free environment or keep away from any sources of allergy.
Treatment
- Early recognition of allergic reaction.
- An early call for help.
- Immediate first aid measures.
- Avoidance of allergens.
Health Teaching
- Patient’s need to know the allergens and how to avoid it.
- Patient and family need to recognize the early symptoms and how to manage it.
- Importance of early detection and management.
- Avoid contact with allergens.
Out-patient Care
- Adherence to follow up consultation after confinement.
- Referral to specialist.
Diet
- Hypo-allergenic diet.
- Eat organic foods, fruits, meats and vegetables, whenever possible.
- Avoid anything with sugar, glucose, fructose, EDTA, MSG, flavoring, color, or other additives or preservatives.
- Provide a hypo-allergenic food guidelines or what foods to eat and what foods to avoid.
Statistics shows that anaphylaxis mortality rate is low and stable, despite the increasing prevalence—but, its irreversible damage and the life-long disability which can occur after anaphylactic shock can never be ignored. The emergency state of anaphylactic shock remains to be an alarming truth of disability causing financial, physical and emotional burden. The reaction occurs without any warning and can be a frightening experience for those at risk and for their families.
The most important requirements in the treatment of anaphylactic shock are early detection, early diagnosis and immediate interventions without any delay of each procedure. The aim of resuscitation is to restore and maintain the vital organ perfusion and prevent complications of irreversible damage. Thus, the patient and family should be aware of the condition and knowledgeable on immediate first aid measures before the patient reach health care facilities. Health care providers such as physicians, nurses, and other anxillary health teams should be knowledgeable enough with proper training and expertise in handling emergency situations like anaphylactic shock. They should base their decisions on both clinical situations and comprehensive advance knowledge on the pharmacologic background and the rationale of every intervention.
“Time counts to save the patient on the impending doom of anaphylactic shock.”
References:
- Spectrophotometer, Decreases Independently of Venoconstriction During Hepatic Anaphylaxis in Perfused Rat Liver. Shock, 26(1), 62–68. Decker, W.W. et al (2008).
- The Etiology and Incidence of Anaphylaxis in Rochester, Minnesota: A Report from the Rochester Epidemiology Project. Journal of Allergy and Clinical Immnunology, 122(6), 1161–1165.National Highway Traffic Administration (1990). Emergency Medical Technician-Basic:
- National Standard Curriculum Instructor’s Course Guide. United States Department of Transportation. Scanlon, V.C. & Sanders, T. (2007). Essentials of Anatomy and Physiology, 5th ed. Philadelphia: F.A. Davis Company, 327–336. Sheikh, A. et al (2012).
- Adrenaline (Epinephrine) for the Treatment of Anaphylaxis With or Without Shock (Review). The Cochrane Library, 4: JohnWiley & Sons, Ltd. http://summaries.cochrane.org/CD006312/adrenaline-for-the-emergency-treatment-of-anaphylaxis Sheir, D.N. et al (2006). Hole’s Essentials of Human Anatomy & Physiology, 9th ed. New York: McGraw-Hill Companies, Inc. Smeltzer, S.C. & Bare, B.G. (2004). Brunner & Suddarth’s Textbook of Medical-Surgical
- Nursing, 10th ed. PA: Lippincott Williams & Wilkins, 296, 311–312. Soar, J. et al. (2008). Emergency Treatment of Anaphylactic Reactions—Guidelines for Healthcare Providers. Resuscitation, 77(2), 157–169. Zhao, Z. et al (2007). Head-Down Tilt Posture Attenuates Anaphylactic Hypotension in Mice and Rats. Journal of Physiological Sciences, 57(5), 269–274.




This website is very interesting