Every individual on Earth, regardless of race, economic status, gender or social status does the same thing every single minute to live – that is to breathe in air. But did you know even how natural and fundamental the process of breathing is, its purpose was unknown to humanity for a long time?
It was around the 19th century when scientists started to understand its importance by circling life processes on cells. Breathing supplies the required oxygen to cells and removes excess carbon dioxide from the body – making it an integral part of the metabolic process. Breathing difficulties result in cellular problems and later on death. This is the main reason why during emergent situations, AIRWAY is always a priority.
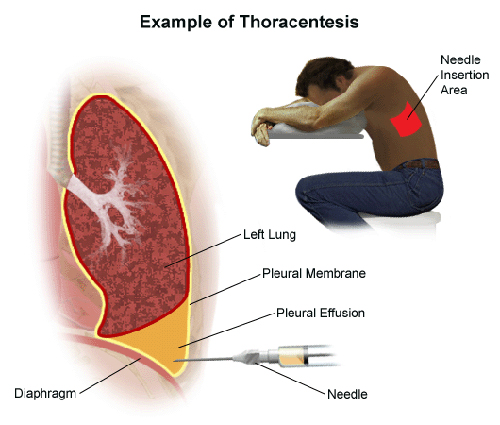
Among other reasons, some clients experience breathing difficulties due to the presence of excess fluid in the pleural space (the space between your chest wall and lungs). Normally, this space contains about 4 teaspoons full of fluid. Excess fluids brought about by lung infections, tumors, heart failure and injury can lead to pleural effusion – the accommodation of fluid in the chest or lungs. Pleural effusion makes breathing taxing and difficult.
To make breathing effortless again, the fluid should be removed from the pleural space. This is where thoracentesis comes into the picture. By definition, thoracentesis is the aspiration of fluid or air from the pleural space. It relieves respiratory distress or pulmonary compression by removing those excess fluid or air resulting from the causes mentioned above.
Furthermore, thoracentesis allows health professionals to obtain specimens of pleural fluid or tissue for analysis. This procedure is also important in the instillation of chemotherapeutic agents or other medication of pleural agents in the pleural space.
Purpose of Performing Thoracentesis
This procedure is performed on clients with various clinical problems. The procedure can either be diagnostically or therapeutically for the:
- Removal of fluid and air from the pleural cavity
- Diagnostic aspiration of pleural fluid
- Pleural biopsy
- Instillation of medication into the pleural space
Contraindication of Thoracentesis
Clients with bleeding disorders are contraindicated to undergo this procedure.
What Happens During The Procedure?
Thoracentesis is performed by the physician and is done by inserting a needle and small, flexible catheter (tube) into the pleural space. This is done under the guidance of an ultrasound that gives visualization on the pleural area. The needle and catheter are used to drain the excess fluid in the area.
The procedure takes about 30-45 minutes to complete, however, it takes longer if a large amount of fluid needs to be removed. Post-thoracentesis, a chest x-ray is performed to check the amount of fluid removed and assess the client for signs of complications.
Thoracentesis Nursing Responsibilities
BEFORE The Procedure
- Check if the consent form has been completed and signed.
- Assess client for known allergies, especially to local anesthetic.
- Place patient in the proper position. Proper positioning stretches the chest or back and allows easier access to the intercostal spaces. The nurse can position the client in one either of the following:
- Assist the client to sit on the edge of the bed with the feet supported and arms and head on a padded over-the-bed table
- Assist the patient to straddle on a chair with his or her arms and head resting on the back of the chair
- If the client is unable to assume a sitting position, assist him or her to lie on the unaffected side. Then elevate the head of the bed to 30 to 45 degrees
DURING The Procedure
- Inform the client of the cold sensation to be felt when antiseptic skin solution is applied to the puncture site. A stinging sensation is also felt during the injection of the local anesthesia.
- Instruct the client to refrain from coughing, breathing deeply or moving during the procedure to avoid injury to the lung.
AFTER The Procedure
- After the needle is withdrawn, apply pressure over the puncture site and a small, sterile dressing is fixed in place.
- Place the client on bed rest.
- Obtain post-procedure chest x-ray results. The x-ray verifies that there is no pneumothorax.
- Record total amount of fluid withdrawn, nature of fluid and its color and viscosity.
- If ordered, prepare samples for laboratory evaluation. A specimen container with formalin may be needed if a pleural biopsy is to be obtained.
- Evaluate the patient at intervals for increased respiration rate, asymmetric lung movement, vertigo, tightness in the chest area, uncontrolled cough with blood-tinged mucus, rapid pulse and signs of hypoxemia.
To prevent pulmonary edema and hypovolemic shock after the procedure, fluid is removed slowly and no more than 1000 ml of fluid is removed during the first 30 minutes. Also, it is vital to check the client for complications post-thoracentesis to provide timely interventions.



![Caring for Patients with Tracheostomy and Nursing Diagnoses [ Updates] tracheostomynursingprocedure](https://rnspeak.com/wp-content/uploads/2020/10/tracheostomynursingprocedure_725820712-238x178.jpg)




Can you direct me to scope of care for an RN? Can an RN or CRT remove the catheter? Must an MD be present? Is there a national standard or is it regulated at state or facility level? Thanks.
Thanks alot
Welcome Amazia 🙂