![Cancer Nursing Care Plan and NANDA Guidelines [Updates] 1 CancerNursingCarePlan](https://rnspeak.com/wp-content/uploads/2018/10/CancerNursingCarePlan-nanda-guidelines-1.jpg) Cancer is a potentially fatal disease caused mainly by environmental factors that mutate genes encoding critical cell-regulatory proteins. The resultant aberrant cell behavior leads to expansive masses of abnormal cells that destroy surrounding normal tissue and can spread to vital organs resulting in disseminated disease, commonly a harbinger of Imminent patient death.
Cancer is a potentially fatal disease caused mainly by environmental factors that mutate genes encoding critical cell-regulatory proteins. The resultant aberrant cell behavior leads to expansive masses of abnormal cells that destroy surrounding normal tissue and can spread to vital organs resulting in disseminated disease, commonly a harbinger of Imminent patient death.
Most types of a cancer cells clumps together to form a mass or tumor. When a cell breaks away from the tumor, it can be swept into the lymph system or bloodstream and carried to other parts of the body where new tumors can be formed.
Classifications of cancer
- Lymphomas -cancers originating in infection-fighting organs
- Leukemia’s -cancers originating in blood-forming organs
- Sarcomas -cancers originating in bones, muscle, or connective tissue
- Carcinomas-cancers originating in epithelial cells
Common Signs of Cancer
- A lump or thickening in the breast or testicles are indicative signs for further investigation.
- A change in a wart or mole may be reflective of melanoma or squamous carcinoma.
- A persistent skin sore that does not heal may be indicative of melanoma.
- A change in bowel or bladder habits, such as constipation, chronic
- diarrhea, abdominal pain, rectal or urinary bleeding indicating gastrointestinal cancer.
- A persistent cough or coughing up blood, indicating bronchial tree damage.
- Constant indigestion or trouble swallowing, are common signs of colon, stomach, or esophagus cancer.
- Unexplained weight loss, as cancer cells use up the patient energy source without him/her knowing it.
- Unusual bleeding or vaginal discharge may be signs of uterine, endometrial or cervical cancer.
- Chronic fatigue, a symptom often accompanied by rapidly progressing cancers.
Due to the multiple health issues and problems that a patient with cancer may have in the duration of the disease, you may encounter the need to implement several nursing care plans. These nursing care plan may include but are not limited to:
- Risk for/Fluid Volume Deficit
- Risk for Infection
- Risk for Altered Family Processes
- Readiness for Enhanced Self-Care
- Pain ( Acute, Chronic and Intractable)
- Anxiety
- Knowledge Deficit
- Body Image Disturbance
- Impaired Skin/Tissue Integrity
- Impaired Elimination Pattern
- Fear
- Self-care Deficit
- Alteration in Nutrition: Less than body requirements
- Disturbed Sleeping Pattern
- Situational Low Self-Esteem
- Anticipatory Grieving
These nursing diagnoses are discussed in detail below.
Risk for Infection
Assessing for risks for infection should be a priority among immunocompromised patients. These possible causes (0r related factors, as expressed in NANDA nomenclature) include, but are not limited to:
- Impaired skin integrity;
- Chemical or mechanical damage to the tissues;
- Lack of knowledge on infection control measures;
- Side effects of medications used for therapy;
- Presence of foreign objects (feeding tubes, catheters, IV lines, etc.); and
- Irritating effects of radiation therapy on skin and tissues.
Assessment of the presence of these risks include checking for any breaks in the skin which can serve as an entry of microorganisms that can cause infection. IV lines, catheters and other devices attached to the patient should be disinfected assessed for any breaks, cleanliness or presence of discharges. A thorough assessment will also reveal whether the infection is a problem that is still a risk or already present in the patient.
Possible Nursing Diagnoses and Related Factors
Risk for infection related to inadequate primary defenses (i.e., alteration in skin integrity; mechanical or chemical tissue trauma)
Risk for infection related to immunosuppression/immunosuppressive effects of therapy (i.e., bone marrow transplantation; chemotherapy; radiation therapy)
Risk for infection related to presence of foreign objects in the body (i.e., IV lines; catheters; feeding tubes, etc.)
Risk for infection related to lack of information about proper infection control measures
Note: “evidenced by” is not usually applicable for a risk diagnosis since the presence of signs and symptoms already makes the nursing problem an actual diagnosis.
Desired Outcomes
After nursing interventions, the patient is expected to (choose what is related to the identified risk):
- Reduce the risk of infections;
- Remain afebrile and free from signs of infections;
- Understand different measures to reduce the risk of infections;
- Verbalize knowledge of the signs and symptoms of infection to watch out for;
- Care for infection-prone sites.
Cancer Nursing Care Plan
| Nursing Action | Rationale |
| Assess patient thoroughly for any possible entry point or signs or symptoms of infection regularly (e.g., skin integrity; respiratory system; tubings, etc.) | One of the best means of prevention of infection is to delay the progression of infection and know the usual portal of entry of infection-causing microorganisms. |
| Monitor patient temperature regularly. | Elevation of temperature may occur based on several factors such as intake of medication, disease process, or presence of infection. |
| Encourage good handwashing and demonstrate proper techniques to patient and his significant others. | Handwashing is one of the most efficient ways of preventing infection. |
| Routinely monitor the patient’s white blood cell count, serum protein, and serum albumin. | These laboratory values are closely linked to the patient’s nutritional status and immune function. |
| Emphasize the importance of limiting visitors and exposure to others. | This helps to minimize the possible sources of infection and cross-contamination with others. |
| Promote adequate periods of rest and activity. | This helps limit the fatigue experienced by the patient and helps proper circulation, boosting immune system. |
| For bed-ridden patients, ensure that all linens are kept clean and dry and proper the turning schedules prescribed. | Prevents impairment of skin integrity, development of decubitus ulcers and pneumonia. |
| Limit invasive procedures and/or touching any lines or tubing attached to the patient. Follow aseptic technique. | Aseptic technique reduces the risk of contamination and also limits the portal of entry of infectious agents. |
| Encourage patient to increase fluid intake if not contraindicated. | It helps thin out secretions and replace fluid loss during fever. It also prevents stasis of urine by promoting diluted urine and frequent emptying of the bladder. |
| Wear gloves during any contact with mucus, blood, and other body fluids. Use goggles when appropriate. | It prevents the transfer of microorganisms that are already on the hands and to protect the hands from becoming contaminated. |
Risk for/Fluid Volume Deficit
Fluid volume deficit is another risk factor that the nurse should place in priority for patients with cancer. This is due to the massive nausea and vomiting that the patient is experiencing, especially after chemotherapy sessions. Assessment of the patient for a present or risk problem for fluid volume deficit may yield:
Actual problem for Fluid Volume Deficit
- Poor skin turgor
- Delayed capillary refill time (more than 3 seconds)
- Dried mucus membranes
- Concentrated urine or decreased urine output
- Constipati on
- Alterations in vital signs (increased pulse rate and heart rate, lower blood pressure)
- Alteration in levels of consciousness, especially when the fluid volume loss is severe
Risk for Fluid Volume Deficit (these conditions may be present during assessment)
- Excessive losses
- Vomiting
- Diarrhea
- Increased amount of drainage (i.e., indwelling catheters, suction and drainage tubes)
- Profuse sweating
- Excessive sweating
- Reduced fluid intake/fluid restrictions
- Poor tolerance for oral fluid intake
Possible Nursing Diagnoses
Fluid Volume Deficit
Fluid Volume Deficit related to excessive losses (specify the condition causing the excessive loss) as evidenced by (indicate signs and symptoms seen).
Fluid Volume Deficit related to an inability to take the recommended fluid intake as evidenced by (indicate signs and symptoms seen)
Risk for Fluid Volume Deficit
Risk for Fluid Volume Deficit related to intake less than recommended
Risk for Fluid Volume Deficit related to excessive losses through (indicate if it is vomiting, diarrhea, etc.)
Desired Outcomes
After rendering nursing interventions, the patient is expected to:
- Display adequate fluid balance, as evidenced by (indicate here a reversal of the symptoms that were recorded prior to diagnosis)
- Increase fluid intake to restore appropriate fluid balance
- Reduced, if not eliminate, the risk for fluid volume deficit
| Nursing Action | Rationale |
| Assess the patient’s vital signs, focusing closely on parameters that indicate fluid balance such as: temperature, blood pressure, heart rate, pulse rate.*+ | Vital signs are one of the best indicators of fluid balance. An increased temperature, heart rate and pulse rate coupled with a reduced blood pressure is highly indicative of reduced total circulating fluid volume. |
| Monitor intake and output, including daily weights and record *+. (Include in the monitoring all sources of fluid input such as IV lines, gavage and lavage, etc.).
Daily weights are usually taken at the same time each day, with the patient wearing the same type/fabric of clothing. |
Intake and output records of the patient helps to show if the patient is retaining fluid, or losing more than the expected base on his condition. These values are normally recorded and analyzed over fixed periods of time to determine if the patient is losing fluids, retaining them or if the interventions provided have proven to be effective. |
| Assess the skin turgor of the patient, taking care to obtain findings in areas not easily affected by weight loss or weight gain such as the chest wall.*+ | Skin turgor is one indirect indicator of hydration status of the patient. Tenting of the skin, especially for prolonged periods after the assessment may indicate poor turgor. |
| Identify other parameters such as hematocrit counts, urine specific gravity, and other indicators of fluid balance.*+ | An elevated hematocrit count and urine specific gravity may indicate dehydration, thus confirming the diagnosis. |
| Encourage increased fluid intake up to 3L per day, if tolerated. For patients receiving IV fluids, ensure that proper calibration of the pump is made while infusing. *+ | Increasing fluid intake is one of the best ways to restore adequate fluid balance, and also helps ensure adequate functioning of the renal and cardiovascular systems. In patients receiving cyclophosphamide, increasing fluid intake also helps reduce the risk for development of cystitis. |
| For patients who are able to tolerate oral intake, assess for other possible sources of fluids that he prefers (i.e., popsicles, ice cubes, soup, gelatin, etc.)*+ | Having several choices for fluid source helps in ensuring that the minimum volume of intake is met, and that the patient participates more in his care. |
**NOTE: All interventions marked with asterisks (*) are done for patients with the diagnosis Risk for Fluid Volume Deficit, while entries marked with (+) are implemented for patients with the diagnosis Fluid Volume Deficit.
Risk for Altered Family Processes
Alteration in family processes may occur in patient with cancer because of the change ins roles individuals in a family may face during the disease process. It can be an actual nursing problem or a problem that is at risk for occurring. This is a nursing diagnosis that includes not only the patient, but also sometimes involve family members and significant others.
Assessment
Assessment of the Risk for Altered Family Processes usually reveals the following conditions present:
- Change in communication patterns within the family;
- Varying roles performed by members of the family;
- Disrupted routines in the family;
- Diagnosis of cancer/terminal cancer;
- Potential loss of a loved one due to cancer.
Desired Outcomes
At the end of nursing interventions, the patient and/or significant other is expected to:
- Verbalize feelings about changes in family processes;
- Participate in interventions to help resolve issues;
- Find meaning in the experience that the patient/SO is going through;
- Develop mechanisms needed for coping and adjusting to the current situation.
| Nursing Action | Rationale |
| Observe usual family dynamics between the patient, his family and significant others. Determine the roles that each one plays and how it relates to other members. | This helps the nurse to have an insight on how the current situation affects the family and helps in creating a plan to address the problem. Decision makers in the family usually have a heavier burden as compared to other members. |
| Note for the usual patterns of communication between family members, giving attention to indications of hostility, frustrations and underlying tones of sadness. | Communication patterns is one of the best ways to determine how a situation impacts a family. The nurse should take note of when and in what situations these patterns emerge. |
| Allow the patient/SO to verbalize their feelings about the current situation and how they think it affects them. | Allowing the patient and SO to tell the nurse about their feelings about the situation helps in gauging how it has affected the family. |
| Help the patient/SO explore previous defense and coping mechanisms used for similar situations. | Evaluating the effectiveness of past coping mechanisms used in similar situations help the nurse direct the patient to consider which mechanisms to apply in the current situation. |
| Encourage participation of family members in discussions about feelings and thoughts about the current situation. | The changes in the health status and potential terminal diagnosis of the patient may affect the entire family. Expressing their feelings in front of one another helps in exploring any underlying feelings or issues that may need to be resolved. |
| Guide patients and family members to acknowledge that the situation may be more stressful to them as compared with others. | Knowing which situations bring added pressure or strain to the family helps them in better addressing the issues at hand. This also helps in minimizing denial among family members about the presence of some problems. |
| If needed, refer the family to a therapist or counselor. | Counselors and therapists may help the patient and the family better in terms of exploring possible interventions to address the potential alteration in family processes. |
| Refer to support groups, if needed. | The patient and family can also benefit from joining support groups so that they can also see how others with similar situations are handling the problems. |
Pain (Acute/Chronic)
Pain is defined as an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage (International
Association for the Study of Pain). Acute pain is characterized sudden or slow onset of any intensity from mild to severe with an anticipated or predictable end, and with a duration of less than 3 months. Chronic pain is pain that lasts longer than 6 months.
Assessment
Assessment findings of a patient with pain varies depending on whether it is acute or chronic. Acute pain may be defined or manifested by a combination of the following symptoms:
- Verbalization of feeling pain;
- Decreased attention span or narrowing of focus;
- Guarding behaviors, muscle tension over the affected site;
- Restlessness (especially on patients with moderate to severe pain);
- Changes in vital signs (normally increased BP);
- Pupil dilation;
- Changes or loss of appetite; and others.
On the other hand, patients who are experiencing chronic pain may be seen with the following:
- Changes in sleeping pattern;
- Anorexia;
- Lack of focus or narrowed attention span;
- Decreased ability to perform ADLs;
- (May or may not be present) Report of pain using a standardized scale;
- Isolation from others;
- Irritability;
- Unilateral neglect (usually seen on the affected site).
Nursing Diagnosis
Pain related to biological injuring agent/chemical injuring agent/physical injuring agent (please indicate which is present) as evidenced by (list down signs and symptoms seen).
Desired Outcomes
At the end of the nursing interventions rendered, the patient is expected to:
- Report elimination or reduction of pain perception;
- Increased ability to perform ADLs;
- Use non-pharmacologic means to manage or control pain;
- Participate in pain-reduction interventions;
- Exhibit knowledge and skills required in administering pain control medications.
| Nursing Action | Rationale |
| Assess for pain parameters (PQRST of pain= perception, quality, radiation, severity and time) and document.
Also assess for history of pain, such as recent surgeries and interventions that may increase pain perception. |
The PQRST of pain gives the nurse a picture of how pain is felt by the patient and helps in creating plan to manage it.
Knowing where the pain can possibly come from is helpful in planning care. The nurse gleans a better idea on determining interventions that would not intervene in any care plan being implemented for the patient. |
| Allow patients to verbalize their pain and acknowledge it. | Helps establish trust and rapport between the patient and the nurse, thereby facilitating better care provision. |
| Evaluate and be aware of the painful effects of particular therapies (surgery, radiation, chemotherapy, biotherapy. Include family members in the evaluation. | Some therapies and treatments may cause pain and other discomforts to the patients such as incisions or injections, side effects of certain medications, muscle pains and others. Including the family in this evaluation may also help gather more comprehensive data for use in planning pain management interventions. |
| Provide non-pharmacologic pain management such as, but not limited to: diversionary activities (listening to soft music, watching TV, reading, etc.); massages; hot and cold compresses; positioning properly on bed; guided imagery. | Non-pharmacologic pain management techniques help promote relaxation, enhances the attention span and helps reduce overall pain perception of the patient. |
| Administer pain medications as prescribed.
-NSAIDs -Opioid
Ensure that proper protocols for use and administration of pain medications are followed. |
Various pain medications have different mechanisms of actions that serve to address pain felt by the patient. When administering medications, always note for the correct dosage and frequency, route of administration and potential drug-to-drug or drug-to-food reactions. |
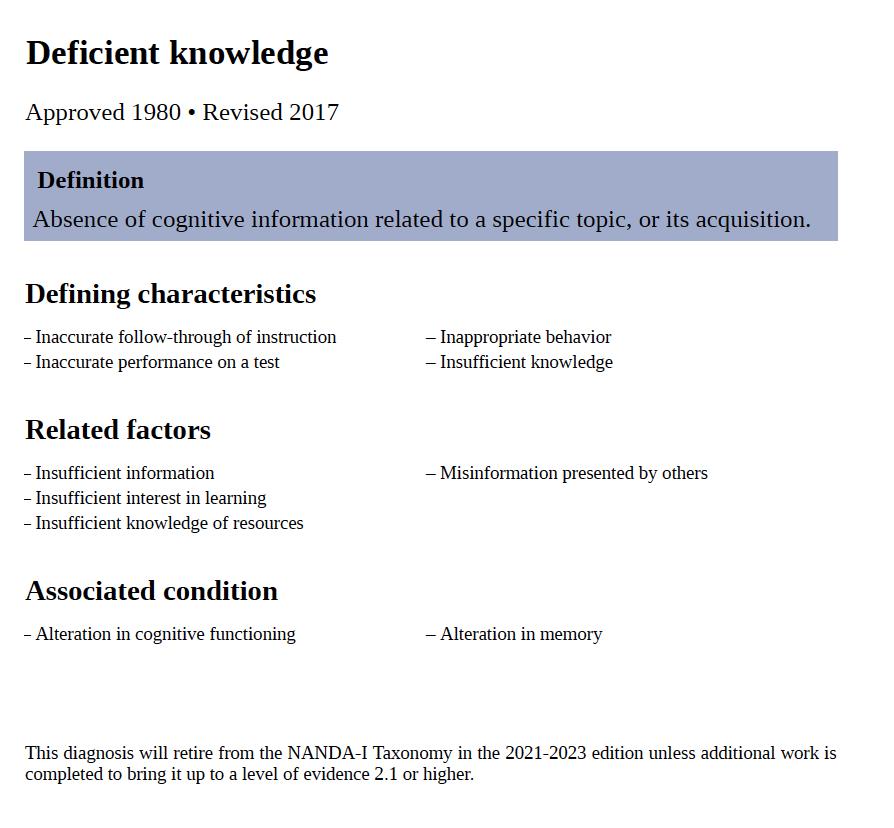
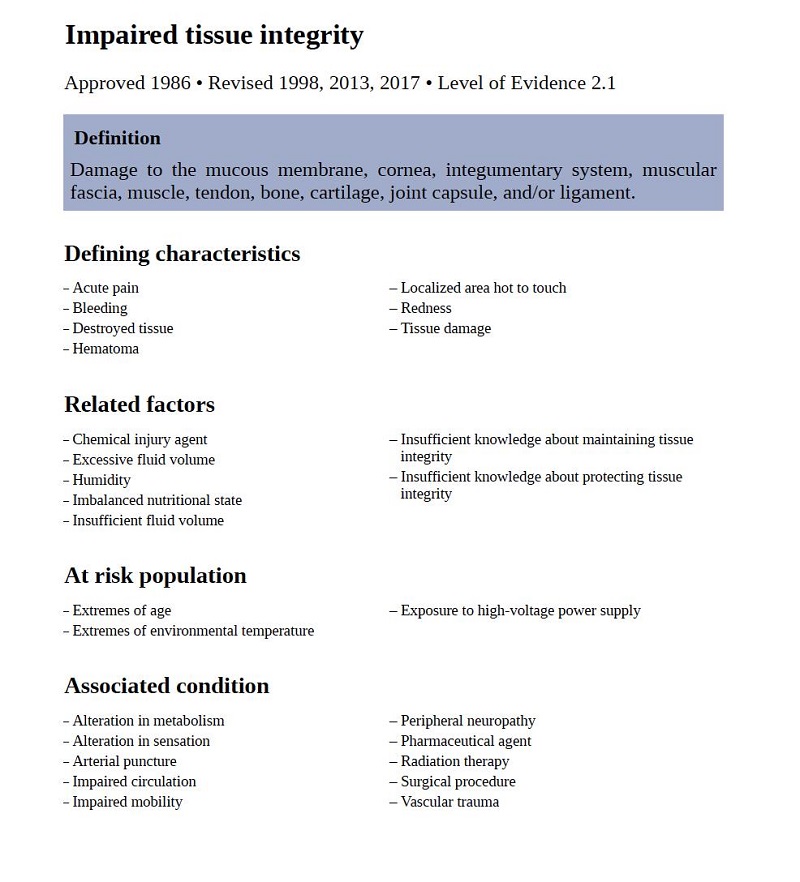
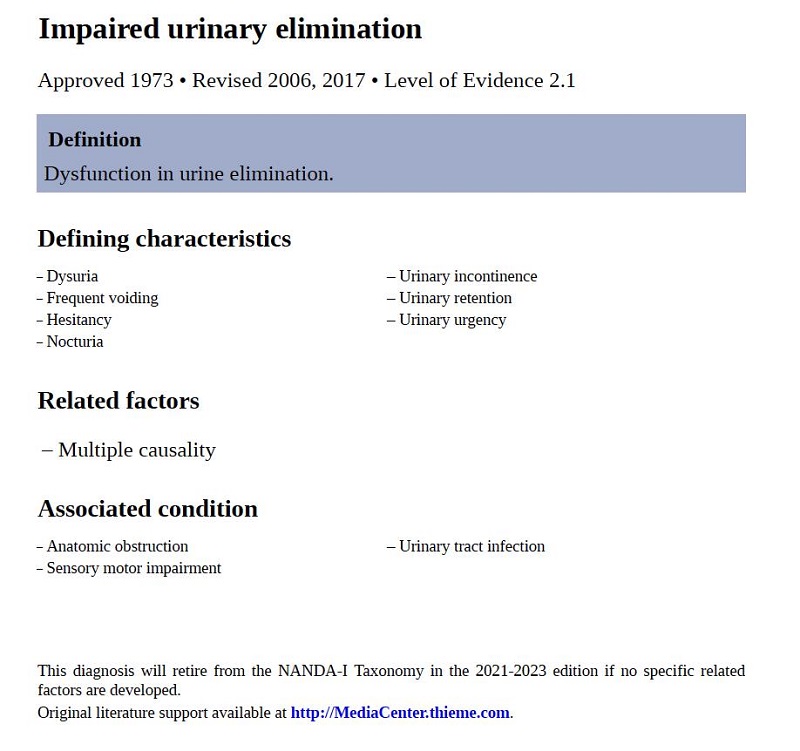
Other Nursing Diagnoses with NANDA 2018-2020 Nomenclature
Knowledge Deficit/Deficient Knowledge
Body Image Disturbance/Disturbed Body Image
Impaired Tissue Integrity
Impaired Urinary Elimination
Anxiety/Fear


![Cancer Nursing Care Plan and NANDA Guidelines [Updates] 2 disturbed body image](https://rnspeak.com/wp-content/uploads/2018/01/disturbed-body-image.jpg)
![Cancer Nursing Care Plan and NANDA Guidelines [Updates] 3 anxiety cancer](https://rnspeak.com/wp-content/uploads/2018/01/anxiety-cancer.jpg)





