Embark on an exciting journey through the complexities of the gastrointestinal (GI) system, which is a remarkable feat of biological ingenuity. This adventure will dive into the structure and functioning mechanisms of the digestive tract’s upper and lower parts. During this analysis, we will highlight the components of the GIT and its various roles, including breaking down food, extracting nutrients, and eliminating waste. Exploring our digestive system in depth will help you develop a deep admiration for its remarkable abilities as it works tirelessly every day to keep us healthy.
The biological structures of the human gastrointestinal system exemplify its complexity and efficiency. Its remarkable workings oversee nutrient extraction and waste elimination, guaranteeing the successful acquisition of necessary sustenance while discarding undesirable components. Let us journey through our digestive machinery to explore this process more deeply.
Healthcare professionals, including nursing students and experienced practitioners, must thoroughly understand the anatomy and physiology of the digestive system. This comprehension is crucial to differentiate between normal physiological processes and abnormal disruptions often seen in medical environments. Furthermore, comprehending the complex architecture and functions of the digestive system is critical to evaluating possible hazards linked with drug intake, application of regional anesthetics, or dealing with gastrointestinal problems such as vomiting. In this discussion, we will delve into a comprehensive investigation of each segment of the digestive tract – starting from the mouth to the anus- analyzing their composition, content, and interconnected mechanisms that transform food into a usable state.
Exploring the Fundamentals of the Gastrointestinal System
The digestive system is a fascinating assembly of organs designed to process food and liquids into usable energy for our bodies while disposing of waste materials. Comprised mainly of the alimentary canal stretching from the mouth to the anus, this complex series of muscles and organs function synchronistically, breaking food down into essential molecules for absorption while expelling useless waste via stool. This wonder system really does great work day in and day out!
The alimentary canal is a conduit for the movement of food and liquids, partially digested through the body’s various organs. This seemingly simple pathway has delicate parts that contribute to its effectiveness – like secretions from hepatocytes, gastric mucosal cells, pancreatic enzymes, and stomach acid. Each component is necessary for nutrient absorption and aiding our bodies natural defense against potentially hazardous substances or pathogens.
An impairment in these areas could dramatically limit the body’s ability to process food and maintain nutrient levels. The gastrointestinal tract is sensitive, and it is essential to remember that digestive conditions can cause severe discomfort or pain if not appropriately treated. This situation should prompt an individual to seek professional medical advice before treatment begins.
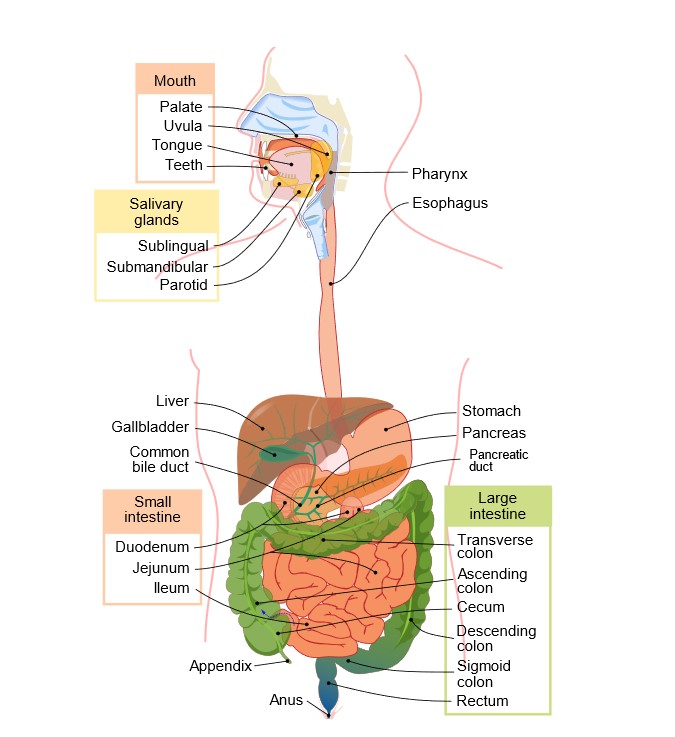
The Digestive Journey Begins: The Role of the Oral Cavity and Enzymatic Action
Digestion commences in the mouth, where food undergoes its first mechanical breakdown through chewing or mastication. This vital step reduces food into smaller and more manageable particles, paving the way for further stages in digestion. The mouth contains crucial digestive components comprising three vital salivary glands: the sublingual, submandibular, and parotid glands. These organs generate saliva, a complex combination of water, mucus, and enzymes. When we chew food, saliva fulfills two roles. One vital function is to moisten the food bolus so that it can be easily swallowed in one go while also starting the process of chemical food breakdown.
The primary process of chemical breakdown involves the digestion of carbohydrates through enzymes. Salivary glands secrete an enzyme called amylase that initiates the procedure of breaking down complicated carbohydrates like starch into more straightforward sugars such as maltose and dextrin. The overall digestion process heavily relies on the crucial roles played by the oral cavity, including the mechanical breakdown of food and the initial enzymatic digestion of carbohydrates. These functions facilitate further digestion and absorption of nutrients in the stomach and intestines.
It’s essential for nurses, especially those responsible for providing nutritional guidance and aid, to have a comprehensive understanding of these mechanisms. Familiarity with the role played by the mouth in digestion can help take care of patients coping with ailments such as the dry mouth or difficulty swallowing – both oral health conditions that can negatively impact nutrient absorption and general well-being.
Understanding the Roles of the Pharynx and Esophagus in Digestion
As the food bolus progresses through the pharynx and into the esophagus, its breakdown – that initially commences within the oral cavity – also continues. Positioned behind both the mouth and nasal cavities, this critical juncture called the pharynx facilitates proper passage of food toward the esophagus while simultaneously initiating swallowing or deglutition.
When food is swallowed, the esophagus undergoes peristalsis – a series of coordinated contractions and relaxations by its muscular walls that help push the food downwards towards the stomach. To aid in this function, the esophagus has longitudinal folds or rugae, making its walls flexible and adaptable to accommodate different sizes of food boluses.
Two functions of digestion are facilitated by peristaltic movements. Firstly, they assist in the physical breakdown of food by processing it effectively with digestive enzymes. Secondly, they promote the conveyance of the partially digested mix known as chyme into the stomach. Therefore, both the pharynx and esophagus have significant responsibilities in ensuring that food travels seamlessly from one end to another within the body.
Nurses must have knowledge about these processes. This knowledge can help them identify and treat issues such as dysphagia, which refers to difficulty in swallowing, and gastroesophageal reflux disease (GERD), which affects the proper functioning of the pharynx and esophagus. Familiarity with the anatomy and physiology of these structures also becomes necessary while managing patients who need enteral feeding or undergo endoscopic procedures.
Decoding the Role of the Stomach in Digestion
The stomach, a vital digestive system component, is crucial in breaking down food particles and aiding their digestion and absorption. It accomplishes this by producing gastric juices through its lining’s gastric glands that contain hydrochloric acid and enzymes. The acidic environment facilitates optimal enzyme activity to efficiently disintegrate food for further processing in the digestive tract, making it possible to absorb necessary nutrients successfully.
Both mechanical and chemical digestion involves the stomach. The body releases gastric juices at the sight and aroma of food, even before it enters the stomach. Within, food mixes with these secretions, mechanically broken down by stomach muscles through churning action, while enzyme pepsin primarily breaks down proteins chemically to aid digestion. The outcome is a semi-liquid form called chyme which gradually moves into the small intestine via the pyloric sphincter. In terms of structure, the stomach can be classified into four primary parts – namely, the cardia, fundus, body, and pylorus. All these sections are essential for digestion in their own singular way. The walls of these segments house specialized cells that create gastric juices, while the potent muscular lining aids in crushing and homogenizing food particles.
Nurses must have a comprehensive understanding of the stomach’s functions and its significance in digestion. This awareness can aid in dealing with medical conditions like peptic ulcers, gastroenteritis, and gastritis. Additionally, it aids them in comprehending the implications of gastrectomy procedures. Moreover, nurses must be conscious of the effects of various medications on stomach function, particularly medicines that influence acid levels, since this may cause disturbances in digestion processes.
Delving into the Small Intestine: The Epicenter of Nutrient Absorption
The digestive system relies heavily on the small intestine, tailored for optimum nutrient extraction. Its surface boasts villi, finger-like projections that are bedecked with even smaller structures known as microvilli. This complex arrangement greatly enlarges the area available for absorption, guaranteeing that nutrients from our diet are absorbed efficiently.
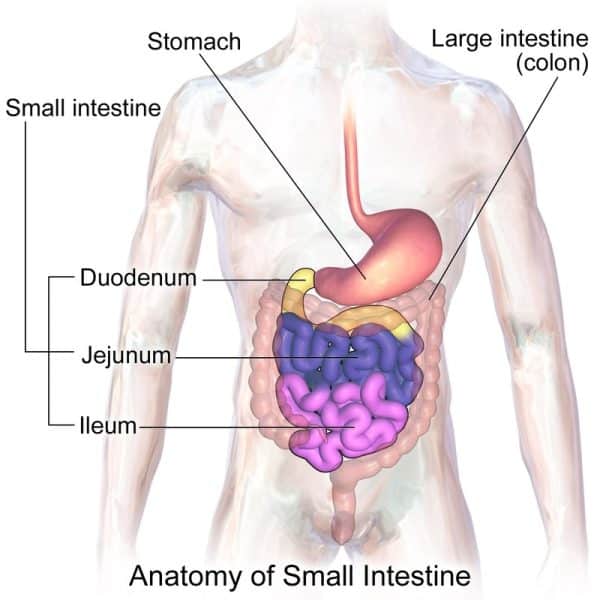
The small intestine is made more efficient by including distinctive cellular structures called Peyer’s patches and Brunner’s glands. Peyer’s patches are clusters of lymphoid tissue that have a crucial role in protecting the body against disease-causing agents that may be present in food entering the gastrointestinal tract. Brunner’s glands, situated mainly in the duodenum, release mucus with abundant bicarbonate ions. The alkaline properties of this secretion help to balance out the acidity levels of chyme from the stomach, creating a favorable environment for digestive enzymes to function correctly.
The three major parts of the small intestine are the duodenum, jejunum, and ileum. The chyme enters the duodenum, where it is mixed with bile and pancreatic juices to help break down carbohydrates, fats, and proteins. Following this process, the jejunum becomes the critical site for absorbing these nutrients. Finally, the ileum absorbs any remaining essential elements like bile salts and vitamin B12, leaving no vital nutrients behind in our body system.
Comprehending the anatomy and physiology of the small intestine is essential for healthcare practitioners, especially nurses. It plays a significant role in managing different medical conditions, such as inflammatory bowel diseases, malabsorption syndromes, and post-surgical care involving the small intestine. Additionally, knowing how various drugs can impact or get influenced the functioning of this organ remains critical in providing excellent patient care and administering medication effectively.
Deciphering the Multifunctional Organ: The Liver
The human body’s largest internal organ, known as the liver, performs various essential tasks, including extracting nutrients and detoxifying. The liver is structured with many small lobules containing hepatocytes, specialized cells responsible for crucial jobs like metabolizing nutrients, removing toxins from the bloodstream, and manufacturing bile – an important digestive substance.
The hepatocytes generate bile which is crucial for the process of digestion. This substance is released into the small intestine, where it assists in breaking down and emulsifying dietary fats, ultimately making it easier for them to be absorbed by the body through the bloodstream.
The liver is a prominent biochemical factory within the body that produces essential compounds such as plasma proteins and nonessential amino acids. It carefully transforms dietary carbohydrates, fats, and proteins into functional forms that can be utilized for energy or structural purposes throughout the body. Additionally, it functions as a detoxification center by filtering out harmful substances, such as drugs and alcohol, from the bloodstream.
The liver plays a vital role in storing essential vitamins and minerals such as iron, copper, magnesium, and B-complex vitamins like B12. Moreover, it produces bile salts critical in digesting and absorbing dietary fats. Therefore, storage is a significant function the liver performs apart from other crucial functions.
In addition, the liver has a crucial function in eliminating toxins from the body. It breaks down proteins, carbohydrates, and fats while removing surplus hormones and other harmful substances from the bloodstream. The detoxification process is facilitated through a sophisticated system of enzymes that convert these compounds into non-toxic metabolites that can be excreted or absorbed again by the body.
In addition to its role in energy production, the liver is also accountable for producing cholesterol, a crucial element needed for creating cell membranes. It’s imperative to keep track of the amount of dietary cholesterol consumed as excessive intake may escalate the susceptibility to contracting ailments such as coronary artery disease.
Exploring the Biliary Duct System and Bile Functions: A Deep Dive
As a vital component of digestion, the liver produces bile, a bioactive fluid. It flows through the biliary duct system and finally reaches the small intestine, breaking down fats and lipids into smaller particles for better absorption. These nutrients are essential in providing energy, growth, and repair of cells within the body. Bile also aids significantly in improving the uptake of carbohydrates, cholesterol, and fatty acids.
Bile possesses a significant alkalinity quality, effectively neutralizing the acidic nature of stomach contents. This increase in pH level helps digestion and enhances the process of breaking down larger molecules into smaller ones that are more easily absorbed by intestinal cells.
The role of bile is not limited to digestion only. It also serves as an effective way to ward off microbes and significantly removes toxins from the body. Thus, it’s imperative to have well-coordinated biliary duct functioning for sustaining good health.
The optimal health of the biliary duct system, a prerequisite for effective nutrient absorption, toxin expulsion, and digestion, necessitates healthy lifestyle habits and a balanced diet. Such practices encourage optimal liver function, critical for producing sufficient bile. Moreover, wise dietary choices aid in modulating bile production and reabsorption in the body, promoting holistic health.
The Finale: Large Intestine
The colon, also known as the large intestine, marks the last phase in the body’s digestive process. Measuring approximately 1.5 meters long, it runs from the ileocecal junction up to the anus and demonstrates exceptional efficiency and specialization in anatomy.
The large intestine comprises several distinct parts, including the cecum, ascending colon, transverse colon, descending colon, sigmoid colon, and rectum. Although each part performs a unique function, they work together to carry out the overall role of the large intestine.
The function of the cecum is to collect chyme from the ileum, marking the beginning of the large intestine’s role. The feces are moved upward by peristaltic movements in the ascending colon, an essential but often neglected step in digestion that requires overcoming gravity.
Involved in absorption and fermentation processes, the longest and most mobile part of the transverse colon mixes digestive residues with the bacterial flora to synthesize vitamins such as vitamin K and specific B vitamins.
As it enters the descending colon, water and electrolytes continue to be drawn out, leading to the gradual hardening of feces. The solidification process persists as it passes through the sigmoid colon, which acts as a reservoir until bowel movement is triggered.
Ultimately, we arrive at the rectum – an essential component in bowel movements that maintains waste until it can be eliminated via the anus.
In terms of the body’s functions, the primary roles of the large intestine include absorbing water and electrolytes, producing vitamins, and converting liquid waste into a solid form. Billions of beneficial bacteria reside in the colon, establishing a mutually beneficial association that promotes intestinal health and boosts the immune system.
Nurses’ understanding of the anatomical and physiological aspects plays a vital role in ensuring proper patient care. Their knowledge about how the colon operates helps them identify various disorders like IBS, diverticulosis, inflammatory bowel disease (IBD), and colorectal cancer, enhancing their ability to aid in early diagnosis and managing these conditions effectively.
Beneath the Surface: GI Tract Wall Structures
The digestive process relies upon the complex construction of multiple layers within the gastrointestinal (GI) tract wall, each layer playing a unique role. The vital function of secretion and absorption in the GI tract is primarily attributed to the innermost layer, called the mucosa. This layer consists of three parts: epithelium, lamina propria, and muscularis mucosae. The epithelium plays a role in absorbing end products of digestion and secreting mucus that has a lubricating effect on the GI tract. The layer that lies beneath the mucosa is referred to as the submucosa. This layer holds blood vessels and lymphatics, which guarantees that nutrients taken in by the mucosa are disseminated throughout the body.
Additionally, it comprises a complex system of nerve plexuses called Meissner’s plexus, which regulates both muscular contractions and secretions generated by the mucosa. The subsequent layer is known as the muscularis externa, which comprises a duo of smooth muscle layers consisting of an inner circular layer and an outer longitudinal layer. This particular stratum is pivotal in gut motility by inducing peristaltic movements that forcefully propel food along the gastrointestinal tract. Within these muscular layers resides Auerbach’s plexus (also referred to as myenteric plexus), dictating the intensity and frequency of muscle contractions during this process. Finally, the serosa layer of the gastrointestinal tract wall, which is located on the outermost part, serves as a protective barrier and fastens the GI tract to adjacent structures.
The Nervous Influence: GI Tract Innervation
The complex and intricate nervous system network, including the enteric nervous system (ENS) – a localized, independent cluster of neurons – and additional innervation from the parasympathetic and sympathetic nervous systems, provides foundational support for the gastrointestinal tract’s functionality.
Through the vagus nerve and the sacral spinal nerves, the parasympathetic nervous system boosts digestion by providing innervation to both the upper gastrointestinal tract up to the transverse colon as well as to the lower part of the colon and rectum. This stimulation increases muscular tone within the GI tract, stimulates peristaltic movements, and triggers digestive enzymes and fluid secretion.
On the other hand, the sympathetic nervous system regulates the actions induced by the parasympathetic nervous system. It decelerates peristalsis and decreases secretion functions, which is a usual reaction during times of pressure or threat to preserving energy in the body.
The enteric nervous system (ENS), which is sometimes referred to as the ‘second brain,’ contains a more significant number of neurons than even the spinal cord and takes charge in independently controlling several GI functions, such as movement, nearby blood circulation, and communication with gastrointestinal, immune cells.
A range of gastrointestinal disorders can occur if any of these systems are disrupted. Nursing professionals must comprehend the complex connections and equilibrium between these neural systems to efficiently evaluate and handle different GI ailments. Understanding these systems emphasizes the significant impact of neural control on digestive health and patients’ overall wellness.
The Dynamic Participants: The Accessory Organs in Digestion
The accessory organs in digestion, namely the liver, gallbladder, pancreas, and biliary duct system, play a crucial role in the digestive process. They are essential components that produce and discharge a range of hormones, enzymes, and bile to aid digestion.
The liver, the largest internal organ, performs various bodily functions, having been identified with over 500 roles. The liver is responsible for metabolism, detoxification, protein synthesis, and clotting factor production. Among its crucial responsibilities in digestion is the synthesis of bile – a substance that facilitates the emulsification and assimilation of fats alongside fat-soluble vitamins.
The gallbladder stores bile generated by the liver and discharges it into the small intestine whenever necessary. Despite its crucial role, a person can survive without a gallbladder. If taken out, the liver can provide bile straight to the small intestine, but this may impact optimal fat digestion. It’s worth noting that even with this organ missing, one can still carry on living normally.
The pancreas has a two-fold role as it functions as an endocrine gland by producing insulin and glucagon that regulates blood sugar levels and as an exocrine gland that secretes digestive enzymes into the small intestine to break down carbohydrates, proteins, and fats.
The biliary duct system comprises multiple tubes which carry bile from the liver to the gallbladder for storage and subsequently to the small intestine, where it is involved in digestion. If there happens to be any hindrance within these ducts, it could lead to severe ailments like pancreatitis or gallstones.
A Final Word: Summary of The Magnificent Complexity of the GIT
The complex arrangement of digestive organs in the body, collectively known as the gastrointestinal system, functions in perfect harmony to meet the nutritional requirements of an individual. Specifically designed to perform specialized functions, each segment begins with food breakdown in the mouth and ends with waste removal through the large intestine, ultimately forming a highly interconnected network of digestive processes.
Oral cavity: Not only does the oral cavity kick-start digestion by physically breaking down food, but it also initiates chemical digestion with enzymes like salivary amylase, which begins the breakdown of complex carbohydrates.
Stomach: The stomach serves as a mixing and storage chamber, churning food with strong muscular contractions and deploying gastric juices that start protein digestion. This combination of mechanical and chemical processing turns the ingested food into a semi-liquid mass called chyme.
Small intestine: This organ, despite its name, has the most extensive surface area due to its villi and microvilli, maximizing nutrient absorption. It’s also where the most substantial part of digestion occurs, with enzymes from the pancreas and bile from the liver further breaking down food components for absorption.
Large intestine: Primarily involved in water and electrolyte absorption, the large intestine houses a vast microbiota that aids in the breakdown of complex carbohydrates the small intestine can’t handle while also producing specific vitamins.
Accessory organs: These include the liver (the body’s metabolic powerhouse), the gallbladder (which stores and releases bile), and the pancreas (which produces digestive enzymes and regulates blood sugar).
In-depth knowledge of the anatomy and physiology of the digestive system is crucial for nursing professionals to effectively aid in the early diagnosis and management of a variety of digestive disorders. Appreciating the remarkable journey that every meal takes through this complex system is a testament to the intricacy and sophistication of human anatomy.
Gastrointestinal System NCLEX Mastery: Conquering Anatomy & Physiology Questions
1. A patient has been diagnosed with hepatocyte damage due to a recent illness. Which of the following functions would be most affected by this condition?
A. absorption of dietary fats
B. Initiation of peristaltic movements in the large intestine
C. Breakdown and removal of toxins from the bloodstream
D. Production and secretion of gastric juices
Answer: C. Breakdown and removal of toxins from the bloodstream
Rationale: Hepatocytes are responsible for several vital functions, including metabolizing nutrients, removing toxins from the bloodstream, and manufacturing bile. While some of these tasks are related to digestion (such as manufacturing bile), their primary role in detoxification would be most affected by hepatocyte damage.
2. Bile, produced by the liver, is crucial for the digestive process. Which of the following best describes its primary function in the body?
A. Assisting in breaking down and emulsifying dietary fats
B. Neutralizing the acidic nature of stomach contents
C. Absorbing water and electrolytes from the chyme
D. Stimulating peristaltic movements in the gastrointestinal tract
Answer: A. Assisting in breaking down and emulsifying dietary fats
Rationale: Bile, produced by the liver and released into the small intestine, primarily helps break down and emulsify nutritional fats. It helps in making these fats more accessible for absorption by the body.
3. The nurse is educating a recently diagnosed liver disease patient about dietary changes. Which nutrients should be monitored closely due to the liver’s role in metabolism?
A. Dietary carbohydrates, fats, and proteins
B. Vitamin D and calcium
C. Water and electrolytes
D. Fiber and simple sugars
Answer: A. Dietary carbohydrates, fats, and proteins
Rationale: The liver plays a crucial role in transforming dietary carbohydrates, fats, and proteins into forms that can be utilized throughout the body for energy or structural purposes. As such, these nutrients should be monitored closely in a patient with liver disease.
4. Which of the following statements best describes the function of the large intestine in digestion?
A. It is the primary site for nutrient absorption.
B. It breaks down food mechanically and chemically into chyme.
C. It absorbs water and electrolytes, produces vitamins, and converts liquid waste into a solid form.
D. It secretes digestive enzymes that break down carbohydrates, proteins, and fats.
Answer: C. It absorbs water and electrolytes, produces vitamins, and converts liquid waste into a solid form.
Rationale: The large intestine’s primary function is the absorption of water and electrolytes, the production of vitamins through the action of colonic bacteria, and the conversion of liquid waste into a solid form that can be excreted from the body.
5. Which of the following correctly identifies the purpose of the muscularis externa layer in the wall of the gastrointestinal (GI) tract?
A. It absorbs end products of digestion and secretes mucus.
B. It holds blood vessels and lymphatics, ensuring the distribution of nutrients throughout the body.
C. It induces peristaltic movements that propel food along the gastrointestinal tract.
D. It provides innervation to the upper and lower gastrointestinal tract, stimulating peristaltic movements and secretion of digestive enzymes.
Answer: C. The muscular externa layer in the wall of the gastrointestinal tract induces peristaltic movements that propel food along the gastrointestinal tract.
Rationale: The muscularis externa is a part of the GI tract wall that consists of two layers of smooth muscle – the inner circular layer and the outer longitudinal layer. This layer induces the peristaltic movements, rhythmic contractions, and relaxations that propel food (bolus) through the GI tract. Option A is incorrect because the absorption of the end products of digestion and the mucus secretion are functions of the mucosal layer. Option B is also incorrect as it is the function of the submucosa to house blood vessels and lymphatics. Option D is incorrect because while innervation does affect peristaltic movements and the secretion of digestive enzymes, it is not the primary purpose of the muscular externa layer itself.
6. A patient has just been diagnosed with cholelithiasis (gallstones), and the nurse provides dietary counseling. Which of the following should the patient be advised to limit in their diet, given the role of bile in digestion?
A. Dietary fiber and simple sugars
B. Dietary carbohydrates, fats, and proteins
C. Vitamins and minerals
D. Fatty and greasy foods
Answer: D. Fatty and greasy foods
Rationale: Bile, produced by the liver and released by the gallbladder, is instrumental in emulsifying and absorbing dietary fats. With gallstones present, bile flow can be hindered, making the digestion of fatty and greasy foods challenging and potentially leading to abdominal pain and discomfort.
7. A nurse is preparing a teaching plan for a patient who recently underwent colectomy surgery. In discussing the absorption of water and electrolytes, which section of the gastrointestinal tract should the nurse emphasize?
A. Small intestine
B. Stomach
C. Large intestine
D. Esophagus
Answer: C. Large intestine
Rationale: The large intestine primarily absorbs water and electrolytes from undigested food. Following colectomy surgery, a patient may have an increased risk of dehydration and electrolyte imbalance due to changes in this absorption process.
8. A patient is complaining of chronic constipation. The nurse knows which part of the colon is primarily responsible for solidifying feces by absorbing water and electrolytes?
A. Ascending colon
B. Transverse colon
C. Descending colon
D. Sigmoid colon
Answer: C. Descending colon
Rationale: The descending colon continues absorbing water and electrolytes, leading to the gradual solidification of feces. Therefore, issues with the descending colon can lead to constipation.
9. The nurse is explaining the pathophysiology of pancreatitis to a patient. The nurse should mention which of the following digestive roles of the pancreas?
A. production of digestive enzymes that help break down carbohydrates, proteins, and fats
B. absorption of end products of digestion
C. Inducing peristaltic movements that propel food along the gastrointestinal tract
D. Synthesis of bile that helps emulsify fats
Answer: A. Production of digestive enzymes that help break down carbohydrates, proteins, and fats
Rationale: The pancreas plays a crucial role in digestion by secreting digestive enzymes that help break down carbohydrates, proteins, and fats in the small intestine. In pancreatitis, these enzymes can activate within the pancreas, leading to inflammation and damage.
10. A nurse is caring for a patient recently diagnosed with Irritable Bowel Syndrome (IBS). The nurse knows that understanding which of the following is crucial to managing the patient’s symptoms?
A. The role of the liver in metabolism and detoxification
B. The function of the pancreas in producing insulin and glucagon
C. The complex and intricate nervous system network that supports the functionality of the gastrointestinal tract
D. The structure and function of the biliary duct system in transporting bile
Answer: C. The complex and intricate nervous system network that supports the functionality of the gastrointestinal tract
Rationale: IBS is often associated with a disruption in the gut’s nervous system regulation. Understanding the complex interactions between the enteric, parasympathetic, and sympathetic nervous systems can provide insight into managing IBS symptoms such as abdominal pain, bloating, and altered bowel habits.
References
- Marieb, E. N., & Hoehn, K. (2019). Human anatomy & physiology (11th ed.). Pearson.
- Martini, F. H., Nath, J. L., & Bartholomew, E. F. (2018). Fundamentals of Anatomy & Physiology (11th ed.). Pearson.
- Neal, M., & Peate, I. (2016). Fundamentals of Anatomy and Physiology: For Nursing and healthcare students (2nd ed.). Wiley-Blackwell.
- Patton, K. T., & Thibodeau, G. A. (2018). Anatomy & physiology (9th ed.). Elsevier Health Sciences.
- Porth, C. M., & Matfin, G. (2019). Porth’s pathophysiology: Concepts of altered health states (10th ed.). Wolters Kluwer Health.